For decades, many people have been told that if a drug is cheap, it must be less effective. That belief still lingers - even though generic drugs are scientifically identical to their brand-name counterparts. They contain the same active ingredients, work the same way in your body, and meet the same strict safety standards. Yet, 78% of doctors say their patients still worry that generics won’t work as well. Why? It’s not about science. It’s about psychology.
Why Do People Still Doubt Generic Drugs?
It’s not that people are irrational. It’s that brand names have been engineered to feel trustworthy. Think about it: you see a brightly colored pill with a memorable name like "Lipitor" or "Zoloft," and your brain links that image to quality, reliability, even prestige. Generic drugs? They’re often white, plain, labeled with a chemical name like "atorvastatin" or "sertraline." No logo. No marketing. Just a price tag that’s 80% lower.
That difference isn’t accidental. Brand-name drug companies spent billions on advertising, packaging, and patient support programs. Generics? They were never meant to compete on emotion. But in 2025, that’s exactly what needs to change.
Here’s the hard truth: if you take a generic blood pressure pill today, it’s just as likely to keep your pressure under control as the brand version. Same for diabetes meds, antidepressants, even cancer treatments. But patients still switch back to expensive brands when they can afford it - not because the generic failed, but because they fear it might.
The Rise of Complex Generics and Biosimilars
Generics aren’t just tablets anymore. In 2025, the FDA approved six new biosimilars for denosumab - drugs used to treat osteoporosis and bone cancer. These aren’t simple copies. They’re complex biologic drugs made from living cells. Getting them right requires labs that cost hundreds of millions to build. And yet, they cost 15-30% less than the original.
Companies like CivicaScript are now producing specialty generics - injectables, infusions, and other high-cost drugs - in U.S.-based facilities. Why? To fix supply shortages. In 2025, there were still 270 active drug shortages in the U.S., many of them for essential medications like insulin or chemotherapy agents. By bringing production home, these companies aren’t just saving money. They’re building reliability.
And that’s the key shift: moving the conversation from "cheap" to "trusted." When a hospital pharmacy uses a generic chemotherapy drug that’s made in Ohio, not India, and it arrives on time, every time, patients start to notice. Trust isn’t built with ads. It’s built with consistency.
How Technology Is Rewriting the Narrative
Imagine scanning a pill bottle and seeing a live blockchain record showing every step of its journey: where the active ingredient was made, who tested it, when it was packaged, and even the temperature it was stored at. That’s not science fiction. It’s happening now.
AI-powered tracking systems are being rolled out in hospital pharmacies to verify the authenticity of generic drugs. Patients can access this data through their provider’s portal. No marketing fluff. Just facts. And for people who’ve been burned by counterfeit meds overseas, that transparency is powerful.
One pilot program in a major Australian hospital gave patients access to this data before they filled a generic prescription. Within six months, patient concerns dropped by 40%. Not because they were told to trust it - because they could see it.
Education That Actually Works
Brochures and pamphlets don’t change minds. Real conversations do.
A 2025 pilot by the American Medical Association trained doctors to have five-minute conversations with patients about generics. Not a lecture. Not a sales pitch. Just: "This is the same medicine. It’s been tested on tens of thousands of people. It’s cheaper because we don’t spend millions on TV ads. Would you like to try it?"
The result? A 35% drop in patient resistance. The biggest change? When doctors said, "I prescribe this to my own family," trust jumped. People don’t trust labels. They trust people.
Pharmacists are now being trained to do the same. Instead of just handing over a bottle, they’re asking: "Have you taken this before? What concerns do you have?" That simple shift turns a transaction into a conversation - and a conversation into confidence.
Why Cost Alone Isn’t Enough Anymore
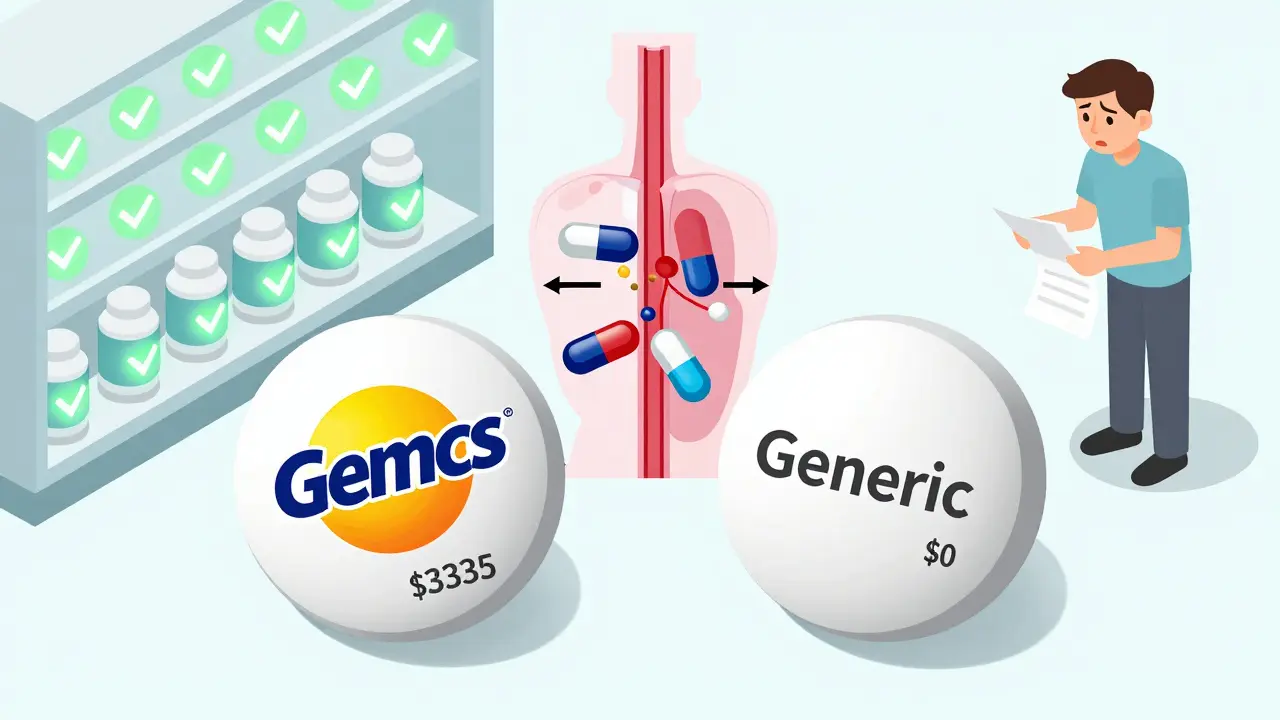
For years, the argument for generics was simple: they save money. And they do. In the U.S., generics make up 90% of prescriptions but only 12% of drug spending. That’s a $300 billion annual savings.
But in 2025, that argument is fading. Why? Because prices are stabilizing. As more manufacturers enter the market, the race to the bottom is ending. Experts like Dr. John Eberle from CivicaScript say generic pricing will soon hit a floor - not because companies are greedy, but because making high-quality drugs costs money. You can’t cut corners on sterile injectables or biologics.
So the new value proposition isn’t "cheaper." It’s "reliable, transparent, and safe." And that’s a message that resonates more than any discount ever could.

The Bigger Picture: Chronic Disease and Systemic Change
More people than ever are living with chronic conditions - diabetes, heart disease, arthritis, depression. These aren’t short-term fixes. They’re lifelong treatments. And for someone on a fixed income, paying $500 a month for a brand-name drug isn’t a choice. It’s a crisis.
That’s why Medicare Part D reforms in 2025 now require insurers to prioritize generics unless there’s a clear medical reason not to. Hospitals are being incentivized to use generic injectables in oncology units - not just to save money, but to treat more patients. One cancer center in Texas reported that switching to a generic version of a chemotherapy drug allowed them to offer treatment to 17 additional patients last year.
And it’s not just the U.S. Countries like Australia, Canada, and Germany have long had strong generic adoption. Their patients don’t question efficacy. They just ask: "Is it covered?"
What’s Next? The Future Is in Trust, Not Price
The next wave of change won’t come from lower prices. It’ll come from better stories.
Imagine a world where:
- Your doctor shows you a side-by-side lab report proving your generic is identical to the brand.
- Your pharmacy app lets you track your pill’s journey from factory to shelf.
- Your insurance plan doesn’t just cover generics - it rewards you for choosing them.
- Generic drugs have names that feel familiar, not clinical - like "CardiAid" instead of "atenolol."
That’s not fantasy. It’s already starting. Companies are testing branded generics - not to inflate prices, but to build recognition. A generic version of a heart medication called "HeartSure" is now available in Australia. It’s still 85% cheaper than the brand. But now, patients recognize it. They remember it. They trust it.
The future of generic drugs isn’t about being the cheapest option. It’s about becoming the most trusted one.
What You Can Do Today
If you’re on a generic medication and you’re still unsure:
- Ask your pharmacist: "Can you show me the FDA bioequivalence data?" They’ll have it.
- Ask your doctor: "Have you prescribed this to your own family?" Their answer matters more than any ad.
- Check your pharmacy’s app or portal. Many now show where your drugs come from and who tested them.
- If you’ve had a good experience with a generic, tell someone. Word of mouth still beats any marketing campaign.
Generic drugs aren’t second-rate. They’re the quiet heroes of modern medicine. They let people live longer, healthier lives without going broke. The only thing holding them back is an outdated idea - one we can all help change.
Are generic drugs really as effective as brand-name drugs?
Yes. By law, generic drugs must contain the same active ingredients, in the same strength and dosage form, and work the same way in your body as the brand-name version. The FDA requires them to meet the same strict standards for quality, safety, and effectiveness. Studies consistently show no meaningful difference in outcomes between generics and brands.
Why do some people feel generics don’t work as well?
It’s mostly psychological. Brand-name drugs come with polished packaging, advertising, and patient support programs that create a sense of trust. Generics are often plain, unlabeled, and cheap - which makes people assume they’re inferior. But the medicine inside is identical. Studies show that when patients understand this, their concerns drop significantly.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs, like pills for blood pressure or cholesterol. Biosimilars are highly similar versions of complex biologic drugs - like injections for cancer or autoimmune diseases. They’re not identical because they’re made from living cells, but they’re proven to work the same way. Biosimilars typically save 15-30% compared to the original biologic.
Are generic drugs safe if they’re made overseas?
Yes - as long as they’re approved by the FDA or equivalent agencies like Australia’s TGA. The FDA inspects foreign manufacturing sites just like U.S. ones. In fact, most generic drugs - even those sold in the U.S. - are made overseas. What matters is regulation, not location. New initiatives like CivicaScript’s U.S.-based production aim to improve supply reliability, but safety standards remain global.
Why are generic drug prices stabilizing?
As more manufacturers enter the market, prices initially drop sharply. But once they hit the cost of high-quality production - especially for complex injectables or biosimilars - prices stop falling. Companies can’t keep cutting costs without risking safety or supply. Experts say this stabilization means the focus is shifting from "lowest price" to "most reliable and transparent."
How can I be sure I’m getting a real generic drug?
Look for the FDA-approved generic label on the bottle. You can also check the FDA’s Orange Book online or ask your pharmacist for the National Drug Code (NDC). Many pharmacies now use digital tracking systems that show where your drug came from and who tested it. If you’re ever unsure, ask your pharmacist to show you the documentation - they’re required to provide it.
Will switching to a generic drug affect my treatment?
For most people, no. Generic drugs are required to be bioequivalent - meaning they work the same way in your body. However, if you’re taking a narrow-therapeutic-index drug (like warfarin or thyroid medication), your doctor may monitor your levels more closely when switching. But this isn’t because generics are less effective - it’s because small changes in blood levels matter more with these specific drugs.
Why aren’t all drugs available as generics?
Patents protect brand-name drugs for 10-20 years. Once they expire, generics can enter the market. In 2025-2027, over 100 major brand-name drugs will lose patent protection, opening the door for generics. Some complex drugs, like biologics, take longer to copy due to technical challenges. That’s why biosimilars are now being developed - they’re the next wave of affordable alternatives.



Katy Bell
November 22, 2025 AT 13:19I used to refuse generics until my dad had to switch to one for his cholesterol med. He was convinced it wouldn’t work - then he got his bloodwork back and his numbers were better than ever. Turns out his anxiety was the only thing failing. Now he jokes that the white pill has more personality than the fancy blue one.
Ragini Sharma
November 23, 2025 AT 01:13so like… why do generics even look so sad?? like imagine if your antidepressant was called ‘sertraline’ instead of ‘zoloft’… it’s basically the difference between a Nike sneaker and a plain white sock with a price tag. no wonder people panic.
Ross Ruprecht
November 24, 2025 AT 13:22Bro why are we even having this conversation? It’s medicine, not a fashion brand. If it works, it works. Stop paying for logos.
Bryson Carroll
November 25, 2025 AT 14:46People are dumb and that’s why big pharma wins. They’ve conditioned us to equate price with quality like we’re still living in the 1800s. I once saw someone refuse a generic insulin because it didn’t have a ‘premium’ bottle. That’s not ignorance - that’s a cult.
Dalton Adams
November 26, 2025 AT 17:22Genius idea about branded generics like ‘HeartSure’ - if you’re gonna fight perception, give it a name people can remember. I’d take ‘CardiAid’ over ‘atenolol’ any day. It’s not branding - it’s clarity.
Vivian C Martinez
November 28, 2025 AT 03:20I’ve worked in pharmacy for 18 years. I’ve seen patients cry because they couldn’t afford the brand. Then they try the generic and say, ‘Wait… I feel the same?’ That’s the moment trust starts. Not with ads. With results.
Suresh Ramaiyan
November 29, 2025 AT 08:14In India, we’ve been using generics for decades - not because we’re poor, but because we’re practical. My aunt takes a generic blood thinner that costs $2 a month. Her doctor told her: ‘It’s the same as the expensive one, just without the billboard.’ She didn’t need a blockchain to believe him. She needed a human voice.
Kane Ren
November 30, 2025 AT 04:44Love the idea of pharmacists asking, ‘What concerns do you have?’ That’s the missing link. No one wants a lecture. Everyone wants to feel heard. A simple question turns a transaction into a relationship. And relationships build trust - not logos.
Javier Rain
December 1, 2025 AT 22:00Let’s be real - if a drug can save your life and you’re still hesitating because it’s not in a pretty bottle, you’re letting marketing control your health. That’s not smart. That’s surrender. Time to wake up.
Charmaine Barcelon
December 2, 2025 AT 01:41Wait… so you’re saying… people are just… scared… because… the pill is… white???
Laurie Sala
December 3, 2025 AT 08:04I had a friend who switched to a generic antidepressant… and then she said she ‘felt different’… like… emotionally… numb… like… something was off… I mean… what if… it’s not the same??
Vivian C Martinez
December 4, 2025 AT 23:15That’s not the drug. That’s the placebo effect reversing. When people expect to feel worse, they often do - even with identical medication. Studies show that’s why some report side effects with generics that they never had with brands. It’s psychology, not pharmacology.
Lisa Detanna
December 5, 2025 AT 22:49As someone who grew up in a country where generics are the norm, I never understood the stigma. My grandmother took a generic version of her heart med for 12 years. She lived to 94. She never knew what ‘brand’ meant. She just knew it kept her alive. Maybe the real problem isn’t the drug - it’s the culture that tells us we deserve more than survival.
Karla Morales
December 7, 2025 AT 15:44Blockchain tracking? AI verification? 😍 That’s the future. If I can scan my pill and see its entire supply chain - who made it, when it was tested, even the humidity levels in the warehouse - I’m not just trusting a label. I’m trusting data. And data doesn’t lie. 📊✅