When you pick up a prescription and see a different name on the bottle than what your doctor wrote, it’s natural to wonder: Is this the same? Is it safe? Will it even work? You’re not alone. Millions of people in Australia and around the world switch to generic drugs every year to save money, but lingering myths make many uneasy. The truth? Most generic drugs are just as safe and effective as their brand-name cousins. But not all myths are false-and some real risks exist, especially for certain medications.
What Exactly Is a Generic Drug?
A generic drug isn’t a copycat. It’s the exact same medicine, chemically speaking. It has the same active ingredient, strength, dosage form, and way it’s taken (pill, injection, cream, etc.) as the original brand-name version. The only differences? The color, shape, flavor, or inactive ingredients like fillers and dyes. These don’t affect how the drug works in your body.
The U.S. Food and Drug Administration (FDA) and Australia’s Therapeutic Goods Administration (TGA) require generics to prove they deliver the same amount of medicine into your bloodstream at the same rate as the brand. This is called bioequivalence. For most drugs, that means the levels in your blood must fall within 80-125% of the brand’s levels. For high-risk drugs like blood thinners or thyroid meds, the range is tighter: 90-112%.
Manufacturers of generic drugs must follow the same strict quality rules as brand-name companies. In 2022, 98.7% of generic drug factories passed FDA inspections-slightly higher than the 97.3% pass rate for brand-name plants. That means your generic pill is made under the same clean, controlled conditions as the expensive version.
Myth: Generic Drugs Are Cheaper Because They’re Lower Quality
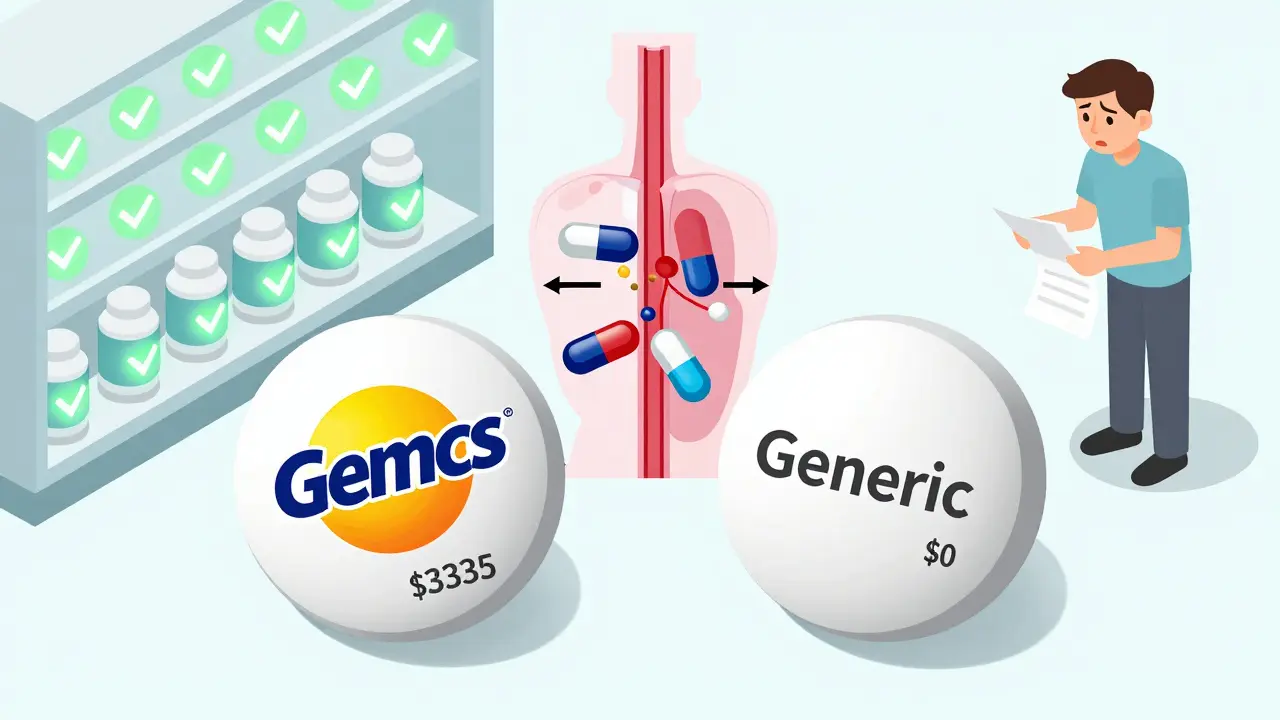
This is one of the most common-and wrong-beliefs. Generics cost 80-85% less because they don’t need to spend millions on research, marketing, or advertising. The original brand paid for those costs to get the drug approved. Once the patent expires, other companies can make the same drug without repeating expensive clinical trials.
They don’t cut corners on the active ingredient. A generic levothyroxine tablet contains the exact same molecule as Synthroid. A generic metformin tablet has the same active compound as Glucophage. The difference isn’t in what heals you-it’s in the packaging and the price tag.
According to the U.S. FDA, generics made up 90.2% of all prescriptions filled in 2021 but accounted for only 19.3% of total drug spending. That’s $2.29 trillion saved in the U.S. alone between 2010 and 2020. In Australia, the PBS (Pharmaceutical Benefits Scheme) relies heavily on generics to keep medicines affordable for everyone.
Myth: Generics Don’t Work as Well
Multiple large studies show generics work just as well-or sometimes better.
A 2020 study in Nature analyzed 17 cardiovascular drugs and found that patients taking generics had fewer heart attacks, strokes, and deaths than those on brand-name versions. For drugs like metformin and gliclazide, the benefit was clear. Another study in 2019 showed generic amlodipine (a blood pressure drug) led to fewer heart-related hospital visits than the brand.
Consumer Reports surveyed 1,200 people who switched to generics. 82% said they noticed no difference in effectiveness. Only 7% reported any change at all.
But here’s the catch: a few specific drugs have shown problems in rare cases. For example, a 2022 study in Epilepsia found patients switching from brand-name Keppra to generic levetiracetam had a 23% higher chance of having breakthrough seizures. One Reddit user reported erratic TSH levels after switching from Synthroid to generic levothyroxine, requiring three dosage changes over six months.
Why? It’s not because the active ingredient is different. It’s because of tiny variations in how the drug dissolves in your body. For drugs with a narrow therapeutic index-where the difference between a helpful dose and a harmful one is small-these small changes matter more.
When Should You Be Careful?
Not all drugs are created equal when it comes to switching. The FDA classifies about 47 drugs as having a narrow therapeutic index (NTID). These include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure control)
- Sirolimus and cyclosporine (organ transplant drugs)
- Carbamazepine and valproic acid (epilepsy and mood stabilizers)
For these, doctors often recommend staying on the same manufacturer’s version-even if it’s generic-because switching between different generic brands can cause fluctuations. Some hospitals and pharmacies now use “dispense as written” rules for NTID drugs to avoid this.
If you’re on one of these, don’t panic. But do talk to your pharmacist or doctor before any switch. Ask: “Is this the same manufacturer as before?” If your blood levels are monitored regularly (like INR for warfarin or TSH for thyroid meds), your provider can catch any changes early.
Why Do Some People Feel Different on Generics?
It’s not all in your head. Some people report side effects, reduced effectiveness, or new symptoms after switching. Why?
First, inactive ingredients. A generic version might use a different dye, preservative, or filler. If you’re allergic to a specific dye-like FD&C Yellow No. 5-you could have a reaction. That’s rare, but it happens.
Second, placebo effect. If you believe generics are inferior, your brain can make you feel worse-even if the drug is identical. Studies show patients who know they’re taking generics report more side effects than those who think they’re on the brand, even when they’re not.
Third, the transition itself. Switching medications-even to an equivalent one-can disrupt your routine. Stress, forgetting doses, or changes in pill size can lead to lower adherence. One 2021 study found adherence dropped by 5.3% in the first 90 days after switching to a generic.
What Do Experts Say?
Dr. Janet Woodcock, former head of the FDA’s drug review division, said: “Generic drugs must have the same quality, strength, purity, and potency as brand-name drugs.” The American Academy of Family Physicians agrees: generics are safe and effective replacements.
But Dr. Aaron Kesselheim from Harvard Medical School adds a crucial note: “Therapeutic inequivalence has been documented in specific cases, particularly for drugs with narrow therapeutic indices or complex delivery systems.”
In other words: for most people, most of the time, generics are fine. But for a small group on critical meds, switching can carry risk. That’s why guidelines exist-and why your doctor or pharmacist should be involved in the decision.

How to Make the Switch Safely
If you’re considering switching to a generic-or already did and feel off-here’s what to do:
- Check the label. Look for the manufacturer name. If you’ve had good results with one generic brand, stick with it.
- Ask your pharmacist. Can they tell you if this is the same as your last bottle? Ask if it’s an NTID drug.
- Monitor your symptoms. If you’re on blood pressure, thyroid, seizure, or mental health meds, keep track of how you feel. Note any new side effects or worsening symptoms.
- Get blood tests if needed. For drugs like warfarin, levothyroxine, or phenytoin, regular lab checks are essential after a switch.
- Don’t assume all generics are the same. Different companies make different versions. If one doesn’t work, ask for another brand.
Most pharmacies automatically substitute generics unless your doctor writes “dispense as written.” That’s legal and common. But if you’re uncomfortable, you can always ask for the brand. Just know it will cost more-and your insurance might not cover it fully.
The Bigger Picture: Why Generics Matter
Without generics, millions of people couldn’t afford their meds. In 2023, the global generic drug market was worth $449 billion. It’s expected to hit $725 billion by 2028. In Australia, the PBS saves patients hundreds of dollars per script every year thanks to generics.
Even the biggest hospitals use generics as their first choice. 98% of U.S. hospitals do. So do most Australian public hospitals. Why? Because they know the science. Generics work.
That said, the supply chain is fragile. Nearly 80% of active drug ingredients now come from China and India. That’s not a problem if quality control stays strong-but it’s why drug shortages still happen.
Final Takeaway: Generics Are Safe-But Stay Informed
For 9 out of 10 people, switching to a generic drug is a smart, safe, and affordable choice. The evidence is clear: they work. They’re not cheaper because they’re weaker. They’re cheaper because the system lets them be.
But for a small group-those on high-risk medications-switching can be risky. That’s not a myth. That’s a fact. And it’s why knowing your drug, asking questions, and monitoring your health matters more than ever.
If you’re on a medication where small changes matter, don’t let cost be the only factor. Talk to your doctor. Get your levels checked. Stay in control. Your health isn’t a trade-off-it’s your priority.
Are generic drugs as safe as brand-name drugs?
Yes, for the vast majority of drugs. The FDA and TGA require generics to have the same active ingredient, strength, and bioequivalence as brand-name versions. Manufacturing standards are identical. In 2022, 98.7% of generic drug facilities passed inspections-slightly higher than brand-name facilities. The only differences are in inactive ingredients like dyes or fillers, which rarely cause issues.
Can generic drugs cause side effects brand-name drugs don’t?
Rarely. Side effects usually come from the active ingredient, which is the same. But if you’re allergic to a dye or filler used in a specific generic version, you could react. That’s why reading the label and checking inactive ingredients matters. Also, some people feel worse simply because they expect to-this is called the nocebo effect.
Which generic drugs should I be cautious about?
Be extra careful with drugs that have a narrow therapeutic index (NTID)-where the difference between a safe and dangerous dose is small. These include warfarin, levothyroxine, phenytoin, cyclosporine, and some seizure meds like levetiracetam. For these, even small changes in how the drug is absorbed can affect your health. Talk to your doctor before switching, and ask for regular blood tests.
Why do some people say generics didn’t work for them?
In rare cases, yes-especially with NTID drugs. Studies have shown higher seizure rates with some generic versions of levetiracetam, and erratic thyroid levels after switching from Synthroid to certain generics. These aren’t common, but they’re real. They’re usually due to slight differences in how the drug dissolves, not because the medicine is fake. If you notice a change, don’t ignore it. Contact your doctor and get tested.
Should I always choose the cheapest generic?
Not always. If you’ve been stable on one generic brand, stick with it. Different manufacturers make different versions, and switching between them-even if both are generic-can cause problems with NTID drugs. Ask your pharmacist if you can refill the same brand. If cost is a concern, most pharmacies offer discount programs or mail-order options for brand-name drugs if generics aren’t working.
Do pharmacists automatically switch me to generics?
Yes, unless your doctor writes “dispense as written” or “no substitution.” This is standard practice and legal in most countries. But you have the right to ask for the brand-name version. If you’re worried about a switch, say so before the prescription is filled. Your pharmacist can help you understand your options.
How do I know if a generic is right for me?
Check if your drug is on the NTID list. If not, you’re likely fine. If it is, talk to your doctor. Ask: “Is there a specific generic brand you recommend?” or “Should I stick with the brand?” Monitor how you feel after switching. If you notice changes in symptoms, energy, or test results, don’t wait-get help. Most people do great on generics. But your health is personal. Don’t assume one size fits all.



Arpita Shukla
November 13, 2025 AT 08:51So many people don't get that generics aren't 'cheap knockoffs'-they're the exact same molecule, just without the marketing budget. I work in pharma logistics in India, and I've seen the factories. Clean rooms, HPLC machines, QA checks every batch. The only difference? No fancy packaging with a logo you recognize. If your thyroid levels are stable on generic levothyroxine, don't fix what ain't broke.
Benjamin Stöffler
November 13, 2025 AT 11:23Let’s be clear: the pharmaceutical industry is a capitalist dystopia-brand-name drugs are a rent-seeking scam, and generics are the proletariat’s rebellion against corporate greed. The FDA’s 80–125% bioequivalence window? That’s not science-it’s a political compromise. And yet… we still take them. We have no choice. Capitalism doesn’t care if your seizure threshold shifts by 0.3 ng/mL. But we do. And that’s the tragedy.
Mark Rutkowski
November 15, 2025 AT 01:04There’s something beautiful about generics. They’re the quiet heroes of modern medicine-no ads, no celebrity endorsements, no inflated stock prices. Just pure, unadorned science doing its job. I’ve been on generic metformin for 8 years. My A1c is steady. My wallet is happy. And I’ve never once felt like I was getting ‘less’ medicine. Sometimes, the most profound things in life are the ones that don’t scream for attention.
Ryan Everhart
November 16, 2025 AT 15:29So… you’re telling me the FDA says 98.7% of generic plants pass inspection? And yet people still freak out when their pill changes color? Interesting. I wonder how many of those people would panic if their iPhone charger changed from white to black. Same specs. Same voltage. Just… different branding. Huh.
David Barry
November 16, 2025 AT 20:04Let’s not sugarcoat this-Australia’s PBS is a miracle, but it’s also a pressure cooker. Pharmacists get paid to swap generics, and sometimes they swap between three different manufacturers in a year. I’ve seen TSH levels swing 3.2 points after a switch from one generic levothyroxine to another. The system works for 90% of people. For the rest? They’re collateral damage. And no one’s auditing the pharmacy supply chain for consistency.
Alyssa Lopez
November 17, 2025 AT 03:04USA is the only country that lets big pharma rip people off. We pay 5x for the same pills. Generics? They’re fine. I switched from Lipitor to atorvastatin and saved $120/month. My cholesterol’s fine. My bank account’s fine. Stop being drama queens. If you’re not in the 2% with NTID drugs, just shut up and take the pill. America needs to stop treating medicine like a luxury brand.
Alex Ramos
November 18, 2025 AT 02:37Big shoutout to pharmacists-they’re the real MVPs here. Last month I switched generics and felt weird, so I called my pharmacy. They checked my script history, saw I’d been on the same brand for 3 years, and held the new batch until I talked to my doc. Seriously, thank you, pharmacy folks. 👏💊
edgar popa
November 18, 2025 AT 16:32Generics work. I’ve been on them for 10 years. No issues. Don’t overthink it. Your body doesn’t care what the label says.
Eve Miller
November 18, 2025 AT 18:21It’s irresponsible to suggest that all generics are interchangeable. The FDA’s bioequivalence standards are a joke. 80–125%? That’s a 45% swing. For a drug like warfarin, that’s not ‘equivalent’-that’s a death sentence waiting to happen. If your doctor isn’t monitoring your INR after a switch, they’re negligent. And the pharmacies? They’re just profit-driven machines. Wake up.
Chrisna Bronkhorst
November 19, 2025 AT 11:04South Africa’s generic supply chain is a mess. We get pills from India, China, even Egypt. Some batches work. Some don’t. I’ve had patients on antiretrovirals crash after a switch. No one tracks which manufacturer they got. No one checks. We’re playing Russian roulette with people’s lives. And no one’s talking about it.
Amie Wilde
November 21, 2025 AT 10:14I switched to generic levothyroxine and felt like a zombie for two weeks. Went back to Synthroid. Energy back. No regrets. My doctor didn’t even blink. Just said, ‘Your body knows what it likes.’
Gary Hattis
November 21, 2025 AT 20:38My grandma in Nigeria takes generic antihypertensives from a local factory. No brand name. No label in English. Just a number and a color. She’s 78. Her BP is perfect. She doesn’t know what bioequivalence means. But she knows her pills keep her alive. Sometimes, the most powerful medicine isn’t the one with the most science behind it-it’s the one you can actually afford to take every day.