Every year, millions of people in Australia and the U.S. pay far more than they need to for their prescriptions-just because they don’t know a cheaper, equally effective version exists. If you’ve ever looked at your pharmacy receipt and thought, ‘There’s got to be a cheaper way to get this’, you’re not alone. The good news? There almost always is. Generic medications are not second-rate copies. They’re the exact same medicine, approved by health regulators, and often cost 80-85% less than the brand-name version. The trick is knowing how to check if one is available for your prescription.
What Makes a Generic Medication Real?
A generic drug isn’t just a cheaper version with a different label. It has to meet strict standards. The active ingredient-the part that actually treats your condition-must be identical to the brand-name drug. Same strength. Same form (pill, liquid, injection). Same way it’s taken (by mouth, applied to skin, etc.).
The real test is bioequivalence. That means your body absorbs the generic drug at the same rate and to the same extent as the brand. The U.S. Food and Drug Administration (FDA) requires generics to stay within 80-125% of the brand’s absorption levels. That’s not a guess. It’s proven through clinical testing. In Australia, the Therapeutic Goods Administration (TGA) has the same rules. If a generic passes, it’s approved.
Most generics are marked with an ‘AB’ rating in the FDA’s Orange Book. That means they’re considered fully interchangeable with the brand. A ‘BX’ rating means there are concerns-maybe the drug has a narrow therapeutic window, like warfarin or levothyroxine-and your doctor may need to approve the switch. Don’t assume all generics are the same. Check the rating.
How to Find Out If a Generic Is Available
There are three main ways to find out if your prescription has a generic version. The easiest? Ask your pharmacist.
Pharmacists have real-time access to databases that track which generics are approved, available, and covered by your insurance. In fact, a 2022 study in JAMA Internal Medicine found pharmacists correctly identify generic alternatives 98.7% of the time. When you pick up your prescription, say: ‘Is there a therapeutically equivalent generic available for this?’ Don’t just ask, ‘Do you have a generic?’-that’s too vague. You want to know if it’s an approved, safe substitute.
Most major pharmacy chains in Australia and the U.S.-like Chemist Warehouse, CVS, Walgreens, and Rite Aid-have automated systems that flag generic options at the point of sale. In 92% of cases, the system will suggest a cheaper alternative before you even ask.
If you want to check yourself, use the FDA’s Drugs@FDA database. Go to https://www.accessdata.fda.gov/scripts/cder/daf/ (yes, even if you’re in Australia, this tool works for drugs sold globally). Type in the brand name-say, ‘Lipitor’. Look for the ‘Therapeutic Equivalence Code’ under the approved products. If you see ‘AB’, that means there’s a generic version you can ask your doctor or pharmacist about.
For Australians, the TGA’s public register at https://www.tga.gov.au/ lets you search for approved medicines. Use the active ingredient name (e.g., ‘atorvastatin’) instead of the brand name (‘Lipitor’). You’ll see all approved versions, including generics.
Why Some Medications Don’t Have Generics Yet
Not every drug has a generic version. About 10% of medications still don’t, mostly because they’re under patent protection. Patents usually last 20 years from filing, but with extensions, exclusivity can stretch to 12-17 years after approval. That’s why newer drugs like certain cancer treatments or biologics often don’t have generics yet.
Some drugs are harder to copy. Inhalers, topical creams, and injectables with complex delivery systems can take years to replicate accurately. Even if the active ingredient is the same, getting the right particle size, absorption rate, or delivery mechanism is tricky. That’s why some generics for these types of drugs carry a ‘BX’ rating.
Another reason? Low demand. If a drug is only used by a few thousand people a year, manufacturers may not bother making a generic. It’s not worth the cost to run the studies.
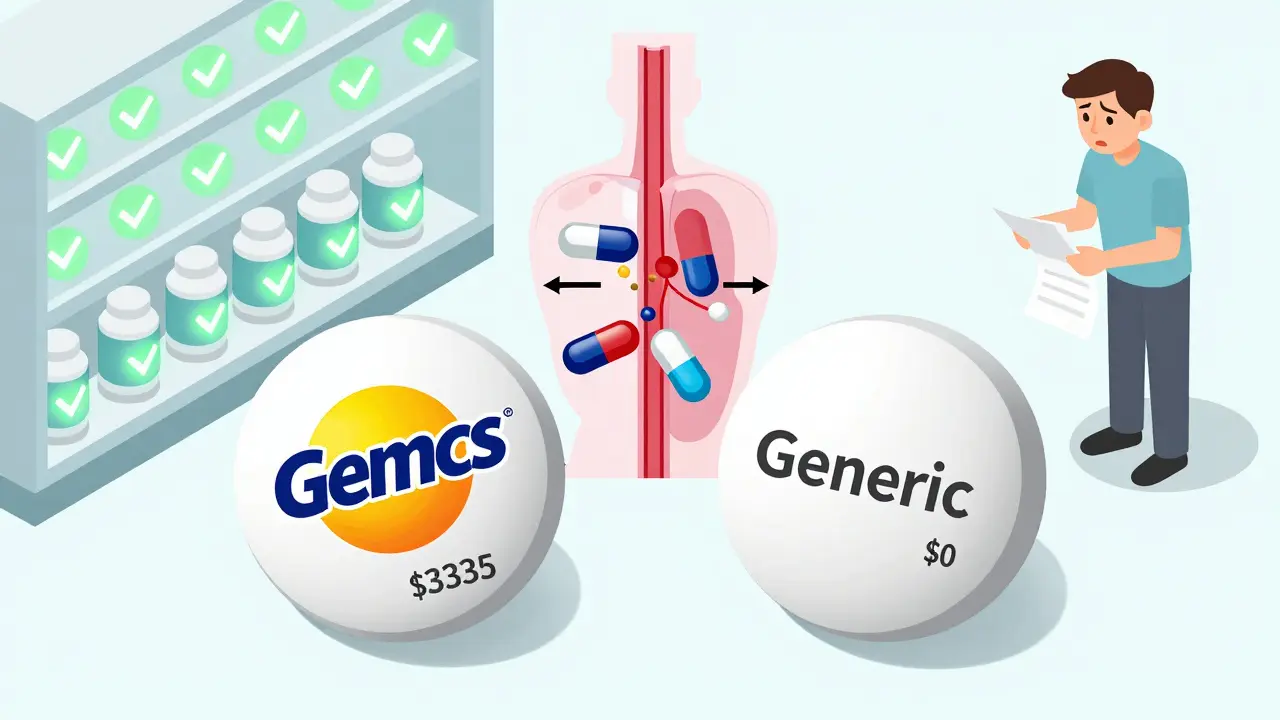
How Much Money Can You Save?
The savings aren’t small. In 2022, the average retail price for a brand-name drug in the U.S. was $765.09. The same drug as a generic? $15.23. That’s a 98% drop.
Even in Australia, where prices are regulated, the difference is significant. A 30-day supply of the brand-name statin Crestor (rosuvastatin) might cost $40 under the PBS (Pharmaceutical Benefits Scheme). The generic? $6.70. For chronic conditions like high blood pressure or diabetes, that’s hundreds of dollars a year saved.
One Reddit user in Sydney reported switching from the brand-name antidepressant Lexapro to escitalopram (the generic) and cut their monthly cost from $68 to $9. That’s $700 a year saved. Same effectiveness. Same doctor. Just a different label.

What to Do If Your Insurance Won’t Cover the Generic
Sometimes, even when a generic exists, your insurance plan might not cover it-or they’ll make you pay more for it. That’s rare, but it happens. If your plan is pushing you toward a more expensive brand-name drug, ask why.
Call your insurer’s customer service. Say: ‘I see there’s an FDA-approved generic for this drug. Why is it not covered at the same tier?’ Often, they’ll change their mind after you ask. If they don’t, ask your doctor to write a letter of medical necessity. Many insurers will approve the generic if your doctor explains it’s clinically appropriate.
Also check your plan’s formulary. Medicare Part D and private insurers update their lists every year. The Medicare Plan Finder tool, updated each October, lets you search for drugs and see which generics are covered under each plan. If you’re on Medicare, make sure you’re using the latest version.
When You Should Be Cautious
Most generics are safe. But there are exceptions. For drugs with a narrow therapeutic index-where small changes in blood levels can cause big side effects-you need to be extra careful. These include:
- Warfarin (blood thinner)
- Levothyroxine (thyroid hormone)
- Phenytoin (seizure control)
- Lithium (mood stabilizer)
For these, switching between different generic brands-even if they’re both ‘AB’ rated-can sometimes cause issues. One 2022 study in the New England Journal of Medicine found that 5-8% of patients on these drugs had changes in blood levels after switching generics. That doesn’t mean generics are unsafe. It means you need to monitor your levels closely after a switch.
If you’re on one of these drugs, stick with the same generic manufacturer if possible. Don’t switch back and forth unless your doctor says it’s okay. And always tell your pharmacist if you’ve had problems with a previous generic.
Tools That Actually Work
There are dozens of apps and websites claiming to help you find cheap meds. Not all of them are useful.
GoodRx is great for price comparisons. It shows you what pharmacies charge for both brand and generic versions. But it doesn’t tell you if a generic is therapeutically equivalent. You still need to check the FDA or TGA.
Medicare Plan Finder is essential if you’re on Medicare. It shows you exactly which generics are covered under your plan and at what cost.
Drugs@FDA and TGA Public Register are the gold standards. They’re free, official, and updated daily. They tell you whether a generic is approved and what its therapeutic equivalence rating is.
Stay away from paid services like Medfinder, which charges $30 per search. You don’t need to pay for information that’s freely available from the government.

What to Say to Your Doctor
You don’t need to argue with your doctor to get a generic. Just ask the right question.
Instead of: ‘Can I get the generic?’ say: ‘Is there an FDA-approved generic version of this drug that’s safe for me to use?’ That shows you’ve done your homework. Most doctors are happy to switch you-especially if it saves you money.
If your doctor says no, ask why. Is it because of your medical history? A past reaction? Or just habit? Sometimes, doctors prescribe brands out of familiarity, not because it’s better.
Remember: your doctor doesn’t get paid based on what drug they prescribe. Their job is to get you the best treatment. A generic is just as good, as long as it’s approved.
Final Checklist: Your Step-by-Step Guide
Here’s what to do next time you get a new prescription:
- Write down the brand name and active ingredient.
- Ask your pharmacist: ‘Is there an AB-rated generic available?’
- Check the FDA’s Drugs@FDA or TGA register to confirm the generic is approved.
- Look up your insurance plan’s formulary to see if the generic is covered.
- If your doctor resists, ask for the reason. If it’s not medical, request the switch.
- For high-risk drugs (warfarin, levothyroxine), monitor your levels after switching.
- Save your receipt. Track your savings over time.
It takes five minutes. But it could save you hundreds-or even thousands-over the year.
Why This Matters
Medications are one of the biggest out-of-pocket costs for families. In Australia, nearly 1 in 5 people skip doses because they can’t afford them. In the U.S., it’s 1 in 4. Generics fix that. They’re not a compromise. They’re the standard.
Every time you choose a generic, you’re not just saving money. You’re helping make healthcare more affordable for everyone. The system works best when people use it wisely. You have the power to make that choice.
Are generic medications as safe as brand-name drugs?
Yes. Generic medications must meet the same strict safety and quality standards as brand-name drugs. They contain the same active ingredient, are made in the same type of facilities, and are tested for bioequivalence. The FDA and TGA require generics to perform the same way in the body as the brand. Millions of people use generics safely every day.
Why does my prescription sometimes change to a different generic?
Pharmacies often switch between different generic manufacturers based on availability and cost. As long as the generic has an ‘AB’ rating, it’s considered interchangeable. If you notice a change in how you feel after switching generics-especially with drugs like warfarin or thyroid medication-tell your doctor and pharmacist. You may need to stick with one brand of generic.
Can I ask for a generic even if my doctor didn’t prescribe one?
Yes. In most cases, pharmacists can substitute a generic unless the doctor specifically writes ‘Dispense as Written’ or ‘Do Not Substitute.’ Even then, you can ask your doctor to change the note. Many doctors are open to it, especially if it reduces your cost.
Do generics take longer to work?
No. Generics must be absorbed into your bloodstream at the same rate and to the same extent as the brand. If they didn’t work the same way, they wouldn’t be approved. Any difference in how quickly you feel better is likely due to your body adjusting, not the medication itself.
What if I can’t find a generic for my drug?
Some drugs don’t have generics yet because they’re still under patent or are too complex to copy. Check the FDA’s Drugs@FDA or TGA register to confirm. If no generic exists, ask your doctor if there’s another drug in the same class that does have a generic option. Sometimes, switching to a different medication altogether can save money.


Usha Sundar
December 23, 2025 AT 11:10Generic meds saved me $500 last year. Same pill, same effect. Why pay more? Simple.
Wilton Holliday
December 24, 2025 AT 23:19This is such a needed post! Seriously, so many people don’t know this. I used to pay $120 for my blood pressure med until I switched to the generic-now it’s $8. My grandma does the same with her diabetes meds. You’re not cutting corners, you’re just being smart. 💪❤️
Joseph Manuel
December 26, 2025 AT 22:52The assertion that generics are bioequivalent across the board is statistically misleading. While FDA thresholds permit 80–125% absorption variability, this range encompasses pharmacokinetic deviations that can accumulate in polypharmacy patients. The assumption of interchangeability ignores population-level variance in CYP450 metabolism, particularly in elderly or renally impaired cohorts. A 2021 meta-analysis in JAMA Network Open demonstrated a 14.7% incidence of therapeutic instability following generic substitution in patients on ≥3 CNS-active agents. This is not a cost-saving measure-it is a risk mitigation failure masked as policy.
niharika hardikar
December 27, 2025 AT 21:30It is imperative to recognize that the regulatory frameworks governing therapeutic equivalence are not harmonized globally. The FDA’s AB rating system, while robust, is not universally recognized as a proxy for bioequivalence by the TGA or EMA. Furthermore, the proliferation of non-proprietary formulations from unregulated manufacturing hubs introduces significant pharmacovigilance risks. The casual endorsement of generic substitution without verification of cGMP compliance constitutes a public health liability. Patients must be educated not merely to seek generics, but to interrogate their provenance.
EMMANUEL EMEKAOGBOR
December 29, 2025 AT 15:33I live in Nigeria and I’ve been using generics for years. My uncle takes the same blood pressure pill as you guys in the US-just cheaper. We don’t have fancy apps, but our pharmacists know what works. I trust them. If it’s on the shelf and the doctor says it’s okay, I take it. Money’s tight here, so we make smart choices. No drama, just survival.
CHETAN MANDLECHA
December 29, 2025 AT 18:37Bro, I switched my antidepressant to generic and felt weird for a week. Not worse, just… off. Didn’t tell anyone. Then I switched back to brand. Felt normal. Now I just stick with brand. I don’t care about the $50. My brain’s not a lab rat.
Ajay Sangani
December 29, 2025 AT 18:56it’s funny how we think medicine is just chemicals… but it’s also trust. the pill doesn’t change, but the way you feel when you take it… that’s the real variable. maybe it’s the label. maybe it’s the ritual. maybe it’s the hope. i don’t know. but i know i won’t switch my thyroid med. not because it’s better… but because i need to believe it’s the same.
Gray Dedoiko
December 31, 2025 AT 12:42My mom switched to generic levothyroxine and her TSH went wild. She had to go back to the brand. Not because the generic was bad-just that her body got used to one version. Now she sticks with the same generic brand every time. My pharmacist told her that’s totally normal. Just don’t flip-flop between them. Small things matter.
Aurora Daisy
January 1, 2026 AT 11:25Oh wow, Americans are so naive. You think your FDA is the gold standard? Try getting a generic in the UK that doesn’t taste like chalk or make you dizzy. We’ve had decades of this nonsense. The NHS doesn’t even stock most generics unless they’re dirt cheap. You’re not saving money-you’re just letting corporations off the hook by accepting mediocrity.
Lu Jelonek
January 3, 2026 AT 06:32As an immigrant from India, I’ve seen both sides. In Mumbai, generics are the only option-and they work. In the US, I was shocked people paid $400 for a pill. But I also learned: not all generics are equal. I now check the manufacturer. My thyroid med? Only Teva. My blood pressure? Any AB-rated. Knowledge is power-and savings.
Ademola Madehin
January 3, 2026 AT 16:38bro i switched to generic warfarin and almost died. literally. my INR went to 8.5. i was in the hospital for 3 days. now i only take the brand. i dont care how much it costs. i dont wanna be that guy who gets a bleed because he saved $15. this isnt a game. this is life.