If you're taking a blood thinner like warfarin, apixaban, or aspirin, and you also take garlic supplements, you could be putting yourself at risk for serious bleeding. This isn't a myth or an old wives' tale. It's backed by real clinical cases, hospital protocols, and peer-reviewed research. The problem isn't garlic in your food-it's the concentrated pills you're popping every day.
Why Garlic Supplements Are Different from Garlic in Food
Eating a clove or two of garlic with your pasta or stir-fry is perfectly safe, even if you're on blood thinners. The amount of active compounds in culinary garlic is too low to cause measurable changes in your clotting. But supplements? They're a different story.Garlic supplements can contain 600 to 1,200 milligrams of concentrated garlic extract per dose. That’s the equivalent of eating 10-20 cloves of garlic in one go. The key player here is a compound called ajoene, a sulfur-based substance that irreversibly blocks platelets from sticking together. Platelets are the cells that form clots to stop bleeding. When they’re inhibited, even minor cuts or internal bruising can turn dangerous.
Studies show that people taking aged garlic extract (like Kyolic, 240mg twice daily) had bleeding times that were nearly 50% longer than those not taking it. Their aPTT-a standard blood test that measures clotting speed-also rose significantly. These aren’t lab curiosities. They’re real, measurable changes that can lead to real bleeding events.
How Garlic Interacts With Common Blood Thinners
Garlic doesn’t just add to the effect of blood thinners-it multiplies it. Here’s how it plays out with the most common medications:- Warfarin (Coumadin): Garlic can push your INR (a key clotting test) higher, increasing bleeding risk. One hospital tracked over 2,300 patients on warfarin and found that those who started or stopped garlic supplements needed INR dose adjustments of 10-25% within days.
- DOACs (apixaban, rivaroxaban, dabigatran): While less studied than warfarin, the risk is still real. Case reports show spontaneous bleeding in patients on these drugs after starting garlic supplements. The European Medicines Agency explicitly warns about this interaction.
- Aspirin and clopidogrel: These are antiplatelet drugs, meaning they also stop platelets from clumping. Garlic does the same thing. When combined, the effect isn’t just additive-it’s synergistic. One study found that 22.4% of patients on these drugs who took garlic supplements developed low platelet counts, compared to just 8.7% in those who didn’t.
The risk isn’t theoretical. Between 2015 and 2022, the National Institutes of Health’s adverse event database recorded 37 cases of serious bleeding linked to garlic supplements and anticoagulants. These included brain bleeds, gastrointestinal hemorrhages, and uncontrolled bleeding during surgery.
Real Cases: When Garlic Nearly Killed Someone
In 2012, two patients scheduled for minimally invasive colon surgery had unexpected complications. Their operations had to be switched from laparoscopic to open surgery because they couldn’t stop bleeding. Their blood tests looked normal. They weren’t on any prescribed blood thinners. But both admitted to taking garlic supplements daily for months to lower cholesterol.Doctors found that the ajoene in the supplements had permanently impaired their platelet function. One patient needed a temporary ileostomy (a bag to collect waste) because surgeons couldn’t safely reconnect the colon. Neither had a history of bleeding problems. Just garlic supplements.
Another case involved a 72-year-old man who had heart valve replacement surgery. He’d been taking ginseng and garlic supplements for years. He bled so badly during the operation that doctors had to stop, transfuse him, and restart. He survived-but only because the surgical team recognized the pattern of herbal-induced coagulopathy.
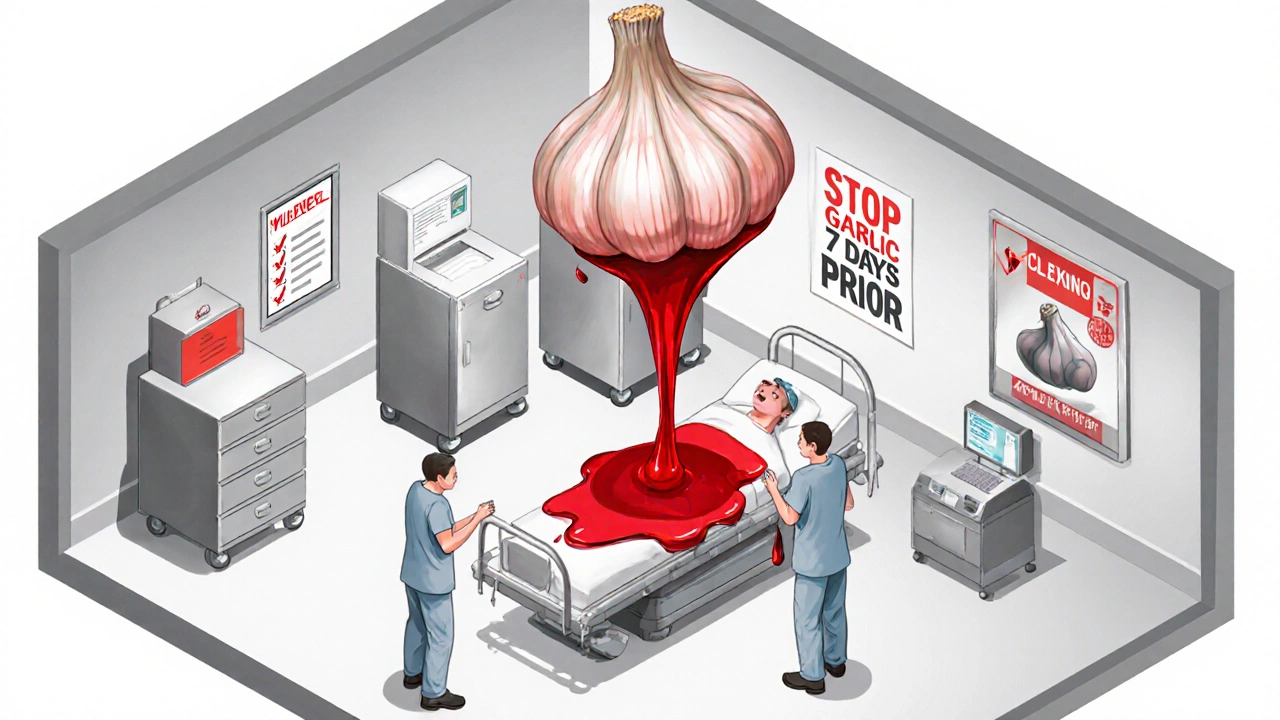
When to Stop Garlic Supplements Before Surgery
If you’re scheduled for any kind of surgery-even a minor one-stop garlic supplements at least seven days before. That’s not a suggestion. It’s a standard protocol from the American Society of Anesthesiologists and the NIH.Why seven days? Because ajoene’s effect on platelets is irreversible. Your body needs that time to make new platelets to replace the ones that are permanently blocked. If you stop only three days before surgery, your blood loss can more than double. One study showed patients who stopped garlic within three days of surgery lost nearly 800mL of blood on average-almost twice as much as those who stopped a week out.
For patients who need emergency surgery and can’t wait, hospitals now use a test called PFA-100. It measures how fast platelets clot under pressure. If the closure time exceeds 193 seconds, surgeons will delay the procedure or give platelet transfusions to compensate.
What About Other Supplements?
Garlic isn’t alone. It’s part of a group of natural products that act like blood thinners:- Fish oil (omega-3s)
- Ginger
- Ginkgo biloba
- Feverfew
- Turmeric (curcumin)
- Red yeast rice
Red yeast rice is especially dangerous. It contains monacolin K, which works just like the statin drug lovastatin. Combine it with garlic and a statin? You risk muscle breakdown (rhabdomyolysis), kidney failure, and even death. The Harvard Medical School team has documented multiple cases of this triple interaction.
The University of California San Diego’s anticoagulation service lists all of these as “high-risk” supplements. They don’t just warn patients-they ask them to sign a checklist before starting any new supplement.

How to Stay Safe
Here’s what you should do if you’re on a blood thinner:- Stop all garlic supplements. Even if you feel fine. The damage isn’t always obvious until it’s too late.
- Don’t assume “natural” means safe. Supplements aren’t regulated like drugs. A 2024 study found that 68% of garlic products don’t even list how much ajoene they contain. Some have none. Others have enough to cause bleeding.
- Tell every doctor and pharmacist you see. Not just your cardiologist. Your dentist, your surgeon, your primary care provider. Many don’t ask about supplements unless you bring it up.
- Use culinary garlic instead. One to two cloves a day is fine. It won’t interfere with your meds.
- Monitor your INR if you’re on warfarin. If you start or stop garlic, get your INR checked within 48-72 hours. Adjustments are often needed.
What’s Being Done to Fix This?
Researchers are pushing for better labeling and standardization. Right now, there’s no way to know how strong a garlic supplement is. One bottle might be harmless. Another could be a ticking time bomb.Two clinical trials are currently underway to measure exactly how aged garlic extract interacts with apixaban. Results are expected by the end of 2024. Meanwhile, the American College of Chest Physicians is drafting new guidelines that may require doctors to screen all anticoagulated patients for supplement use-just like they do for smoking or alcohol.
The message is clear: if you’re on blood thinners, garlic supplements aren’t a harmless addition to your routine. They’re a medical risk. And the consequences can be life-altering-or fatal.
Final Takeaway
You don’t need garlic supplements to protect your heart. Eating garlic in food gives you the flavor and some health benefits without the danger. But popping pills? That’s playing with fire. The science is no longer debatable. The bleeding risk is real. The timing matters. And the consequences are serious.If you’re taking anticoagulants, skip the garlic pills. Stick to the kitchen. Your body will thank you.




jalyssa chea
November 16, 2025 AT 16:58So youre telling me my garlic pills are gonna make me bleed out during a colonoscopy lol
Peter Stephen .O
November 17, 2025 AT 19:47Man i used to pop those garlic capsules like candy thinking theyd lower my cholesterol and boost my immune system turns out i was just playing russian roulette with my platelets
Now i stick to roasted garlic on my toast and i feel way better no weird bruises no weird blood tests just good old food magic
Also shoutout to the doc who caught my INR spiking after i started taking them i thought i was just stressed turns out i was basically self-administering a mild anticoagulant
Julie Roe
November 18, 2025 AT 22:07This is such an important post and i wish more people knew this
I work with elderly patients on warfarin and so many of them swear by their garlic supplements because their cousin in Florida said it cleared their arteries
They dont realize that what works for their cousin might be silently sabotaging their clotting system
And its not just garlic-i’ve seen people on rivaroxaban taking turmeric pills and ginkgo and fish oil like its a smoothie recipe
Doctors dont always ask about supplements and patients dont always think to mention them because they think ‘its just natural’
But natural doesn’t mean harmless
Just because its from a plant doesnt mean your body treats it like a salad
It’s a pharmacologically active compound and it can interact in ways that are silent until its too late
Ive seen patients bleed internally after minor falls because their platelets were already crippled by supplements they thought were ‘safe’
We need better labeling and more public education
Imagine if every supplement bottle had a little red flag that said ‘May increase bleeding risk if on anticoagulants’
Wouldnt that save lives
Also please tell your pharmacist about everything you take-even the ‘tiny’ ones
Theyre the unsung heroes of medication safety
Gary Lam
November 20, 2025 AT 07:18So garlic supplements are basically nature’s aspirin with a side of drama
Meanwhile i’m over here eating a whole head of garlic with my pasta thinking i’m a health guru
Turns out i’m just a culinary ninja and the pills are the real villains
Also why does no one talk about how red yeast rice is just statin in disguise
Thats like buying a fake Rolex and then being mad it doesnt tell time right
Rob Goldstein
November 21, 2025 AT 08:58Just to clarify the mechanism-ajoene irreversibly inhibits the GPIIb/IIIa receptor on platelets which is the same pathway targeted by drugs like abciximab
That’s why the effect lasts days even after discontinuation
It’s not a mild interaction-it’s a pharmacodynamic synergy that can push your bleeding risk into dangerous territory
And yes the PFA-100 test is critical in emergency settings
Many hospitals now screen for herbal supplements pre-op as part of their pre-anesthesia checklist
If you’re on a DOAC and taking garlic you’re not just ‘taking a supplement’-you’re altering your pharmacokinetic profile
And no the label won’t tell you that
Because supplements aren’t regulated like drugs
So it falls on the patient to be informed
And that’s why posts like this matter
Andrew Cairney
November 21, 2025 AT 18:54They dont want you to know this but the FDA and Big Pharma are hiding the truth
Garlic supplements are a natural alternative to blood thinners so they’re trying to scare you off them
Why do you think they pushed this narrative
Also did you know that the NIH database only includes reported cases
There are hundreds of unreported deaths from garlic-induced bleeding
Theyre burying it under ‘unknown cause’
And why do you think they make you stop 7 days before surgery
Because they know how dangerous it is and they dont want liability
And dont even get me started on how they regulate supplements
Its all a scam
Just say no to the system 😡🩸
vinod mali
November 22, 2025 AT 05:03in india we use garlic in every dish but never take pills
my grandma says if you want medicine eat food not pills
she was right
also my uncle took garlic pills for heart and ended up in hospital after tooth extraction
doc said it was the pills
now he eats garlic in curry and lives fine
simple
Kathy Grant
November 23, 2025 AT 16:51There’s something deeply ironic about how we’ve come to distrust food but worship pills
We’ve been conditioned to believe that the more processed something is the more effective it becomes
But nature didn’t design garlic to be crushed into a capsule and swallowed like a vitamin
It was meant to be crushed by a knife on a cutting board, roasted with olive oil, and shared at the dinner table
That’s the ritual that carries the healing-not the pill
And maybe that’s the real message here
It’s not just about bleeding risk
It’s about how we’ve lost touch with the rhythm of real nourishment
We want quick fixes
But the body doesn’t work in quick fixes
It works in rhythm
in patience
in flavor
in connection
Maybe the real antidote isn’t stopping the supplement
But remembering how to eat
Jennie Zhu
November 24, 2025 AT 07:43It is imperative to underscore the clinical significance of this pharmacological interaction. The concurrent administration of garlic supplements and anticoagulant agents constitutes a high-risk, potentially life-threatening combination that necessitates proactive patient counseling and documentation.
As evidenced in peer-reviewed literature, the irreversible inhibition of platelet aggregation via ajoene-mediated pathways significantly prolongs the time to hemostasis, thereby increasing the likelihood of perioperative hemorrhage and spontaneous bleeding events.
Healthcare providers must incorporate structured supplement screening into routine clinical assessments, particularly for patients on warfarin or direct oral anticoagulants.
Furthermore, standardized patient education materials should be disseminated to reinforce the distinction between culinary use and pharmacological dosing.
Failure to do so may result in preventable morbidity and mortality.
Robert Merril
November 25, 2025 AT 11:28so i took garlic pills for 6 months and never had a problem so this is all hype
my friend took them for 2 years and he’s fine
maybe its just me but i think the docs are just trying to sell more blood tests
also why do they say 7 days what if i stop 5 days
im not gonna miss my surgery over a stupid pill
also my bottle said 1000mg but i think its just garlic powder
lol
Gary Lam
November 26, 2025 AT 17:20Bro you just proved the whole point
‘I never had a problem’ doesn’t mean it didn’t happen
It just means you got lucky
And now you’re the reason someone else might not be
Also 5 days isn’t 7 days
Its like saying ‘I only ran the red light for 3 seconds’
Still got hit by the truck
And if your bottle says 1000mg and you dont know what’s in it
Thats not a supplement
Thats a Russian roulette cartridge with garlic flavor