Birth control pills are one of the most common ways women prevent pregnancy-but they’re not as simple as just popping a pill every day. If you’re thinking about starting them, or you’re already on them and wondering if they’re really working, you need to know the real numbers, the real risks, and what can mess them up. This isn’t just about avoiding pregnancy. It’s about understanding how your body reacts, what else might be going on inside you, and how to stay safe.
How Effective Are Birth Control Pills Really?
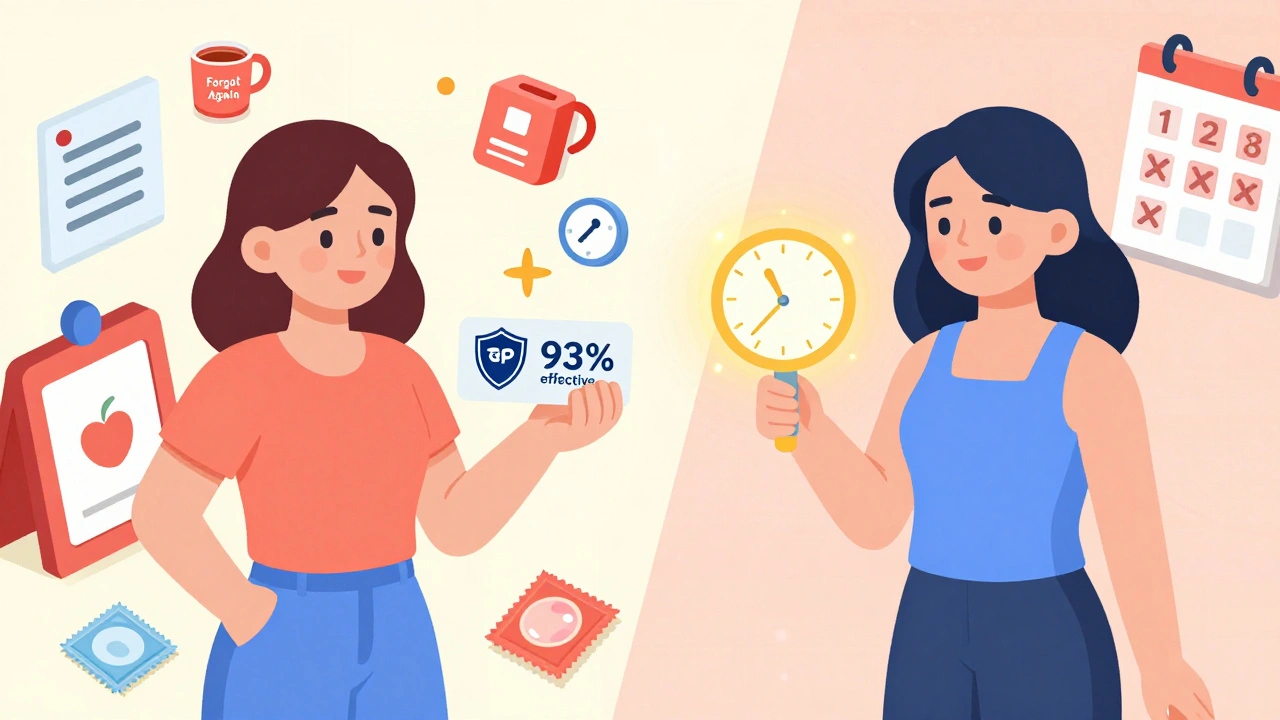
Look up birth control pills online, and you’ll see claims like "99% effective." That number sounds impressive, but it’s misleading unless you know the context. That 99% only applies if you take the pill perfectly-same time every day, no missed doses, no delays. In real life, most people don’t do that. Life happens. You forget. You travel. You get sick. You’re busy.
When you look at how people actually use them-what doctors call "typical use"-the effectiveness drops to about 93%. That means 7 out of every 100 women using birth control pills will get pregnant in a year. That’s not a small number. For comparison, an IUD or implant is 99% effective even with typical use. Those methods don’t rely on daily habits. You put them in once, and they work for years.
Why does this matter? Because if you’re under 21, your risk of unintended pregnancy on the pill is nearly twice as high as someone over 21. Younger users are more likely to miss doses. It’s not about being irresponsible-it’s about routine. Taking a pill at 11 p.m. one night and 8 a.m. the next? That’s not consistent. The hormones need steady levels to block ovulation. When you throw off that rhythm, you’re increasing your risk.
Also, the pill doesn’t work right away. If you start on the first day of your period, you’re protected immediately. But if you start any other time, you need to use a backup method like condoms for at least seven days. Skipping this step is one of the most common mistakes.
What Are the Side Effects?
Side effects vary from person to person. Some women feel nothing. Others notice changes right away. The most common ones are mild and tend to fade after two to three months: nausea, breast tenderness, spotting between periods, headaches, and mood swings.
But there are less common, more serious side effects you need to watch for. These are rare-but they’re real. If you experience:
- Chest pain or shortness of breath
- Severe leg pain or swelling (especially in one leg)
- Sudden vision changes or blurred vision
- Severe headache, especially with confusion or weakness
- Abdominal pain that doesn’t go away
Call your doctor immediately. These could signal a blood clot, stroke, or heart issue. Birth control pills increase your risk of these conditions slightly, especially if you smoke, are over 35, have high blood pressure, or have a history of blood clots.
Modern pills use much lower doses of estrogen than the ones from the 1960s. Back then, pills had up to 10,000 micrograms of estrogen. Today’s pills usually have 20-35 micrograms. That’s a 99% reduction. This change made them safer without losing effectiveness. Still, estrogen increases your risk of blood clots. That’s why progestin-only pills (the "mini-pill") are often recommended for women who can’t take estrogen-like those who smoke, are breastfeeding, or have migraines with aura.
On the flip side, many women use the pill for reasons beyond birth control. It can help with:
- Heavy or painful periods
- Acne (especially pills with drospirenone, like Yaz or Beyaz)
- PMS and PMDD symptoms
- Endometriosis pain
- Reduced risk of ovarian, endometrial, and colon cancer over time
Studies show that after five years of use, the risk of ovarian cancer drops by 27%. After 20 years, endometrial cancer risk is cut in half. These benefits stick around for years after you stop taking the pill.
What Medications and Supplements Can Interfere?
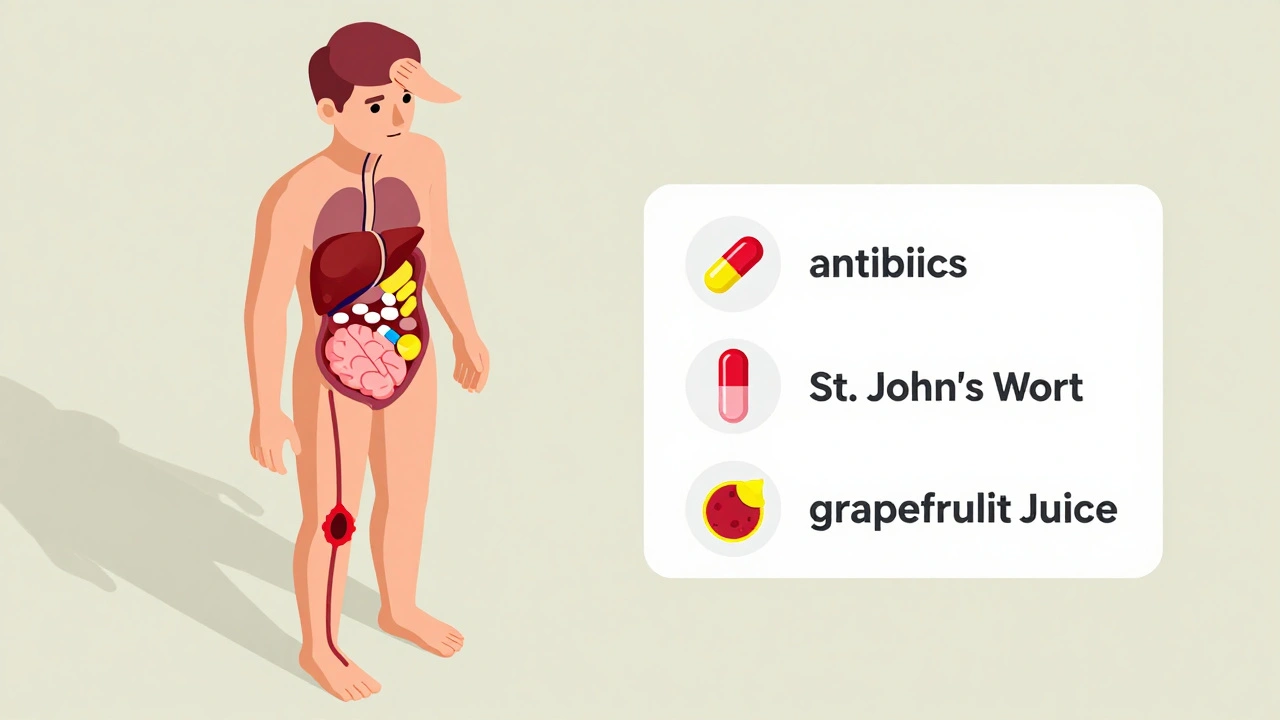
Here’s the part most people don’t know: your birth control pill can be weakened by things you didn’t even think were connected. You’re not just taking a pill-you’re taking a hormone that interacts with your liver, your gut, and other drugs you’re on.
The biggest offender? Antibiotics. Not all of them. But rifampin (used for tuberculosis) and griseofulvin (for fungal infections) are known to make the pill less effective. Most common antibiotics like amoxicillin or azithromycin? The evidence is mixed. But doctors still recommend using backup contraception while taking them, just in case.
Other drugs that can interfere:
- Seizure medications: phenytoin, carbamazepine, topiramate
- HIV medications: efavirenz, ritonavir
- Some antifungals: ketoconazole
- St. John’s Wort
St. John’s Wort is a big one. It’s sold as a natural remedy for mild depression, but it speeds up how fast your body breaks down hormones. That means your pill doesn’t stay in your system long enough to work. Even if you take it "only occasionally," it can still reduce effectiveness.
What about grapefruit juice? It doesn’t make the pill less effective, but it can increase estrogen levels slightly. For most women, that’s harmless. But if you’re prone to blood clots or high blood pressure, it’s worth mentioning to your doctor.
And don’t forget about vomiting or diarrhea. If you throw up within two hours of taking your pill, treat it like a missed dose. Take another pill as soon as you can. If you have severe diarrhea for more than 24 hours, use backup contraception for the next seven days.
Who Should Avoid Birth Control Pills?
Not everyone can safely take them. The American College of Obstetricians and Gynecologists says you should avoid combined pills if you have:
- A history of blood clots, stroke, or heart attack
- Uncontrolled high blood pressure
- Severe liver disease
- Breast cancer or a history of it
- Migraines with aura (visual disturbances, numbness, speech problems)
- Smoking and being over 35
If you’re in any of these groups, the mini-pill (progestin-only) might still be an option. It doesn’t contain estrogen, so it’s safer for many women with these conditions. But it’s also more sensitive to timing-you have to take it within the same three-hour window every day. Miss that window, and your protection drops fast.
Also, if you’re breastfeeding, especially in the first six weeks, estrogen can reduce milk supply. That’s why doctors usually recommend the mini-pill during this time.
What Happens When You Stop?
Some women worry they’ll be infertile after stopping the pill. That’s not true. Fertility returns quickly. Studies show 97% of women have their period back within 90 days of stopping. Many get pregnant within the first month. There’s no "cleanse" period needed. Your body doesn’t need time to "recover."
What you might notice after stopping:
- Return of heavy or painful periods
- Acne flare-ups
- Mood changes
- Changes in libido
If you were using the pill to manage endometriosis or PCOS, symptoms may come back. That doesn’t mean the pill "cured" you-it just masked the symptoms while you were taking it.
How to Use Birth Control Pills Right
If you’re going to use the pill, make it work for you. Here’s how:
- Take it at the same time every day. Set a daily alarm-even if it’s just "pill time."
- If you miss one pill, take it as soon as you remember. If it’s been more than 24 hours, use condoms for the next seven days.
- If you miss two or more pills in a row, take the last missed pill right away and skip the others. Use backup contraception for seven days.
- If you’re sick, vomiting, or on antibiotics, assume the pill isn’t working. Use condoms.
- Don’t skip placebo pills just to avoid your period. That’s fine sometimes, but do it consistently. Talk to your doctor about extended-cycle pills if you want fewer periods.
- Keep a backup method on hand-like condoms or emergency contraception-in case things go wrong.
Apps like Spot On or MyPill can help track doses and send reminders. But don’t rely on them alone. Your phone dies. You forget to check. A paper calendar or alarm is still your best backup.
Is the Pill Right for You?
The pill is great if you want something reversible, non-invasive, and with extra health perks. But it’s not the most effective option. If you’re forgetful, have a busy schedule, or are under 21, consider an IUD or implant. They’re more reliable, require less maintenance, and cost less over time.
If you’re okay with daily routines, want to manage acne or heavy periods, and don’t have any risk factors-then the pill is still a solid choice. Just know the risks. Know the limits. And never assume it’s "working" just because you’re taking it.
And always use condoms if you’re not in a monogamous relationship. The pill doesn’t protect you from STIs. That’s not a side effect-that’s a fact.
Can birth control pills cause weight gain?
Most studies show that birth control pills don’t cause significant long-term weight gain. Some women notice temporary water retention in the first few months, which usually goes away. A 2014 Cochrane review of 49 studies found no consistent evidence that pills lead to weight gain. If you’re gaining weight, it’s more likely due to lifestyle, stress, or other hormones-not the pill itself.
Do I need to take a break from birth control pills?
No. There’s no medical reason to take a break from birth control pills. In fact, stopping and restarting increases your risk of blood clots and unintended pregnancy. Your body doesn’t "get used to" the hormones in a way that requires a reset. If you’re doing well on your current pill, keep taking it unless your doctor advises otherwise.
Can I take birth control pills while breastfeeding?
Combined pills (with estrogen) are not recommended in the first 6 weeks after birth because estrogen can reduce milk supply. After that, if your supply is stable, you may be able to use them-but the mini-pill (progestin-only) is safer and preferred during breastfeeding. It doesn’t affect milk production and is safe for your baby.
What’s the difference between the mini-pill and the regular pill?
The regular pill (combined oral contraceptive) contains estrogen and progestin. The mini-pill contains only progestin. The mini-pill is safer for women who can’t take estrogen-like those who smoke, have migraines with aura, or are breastfeeding. But it’s also more sensitive: you must take it within the same 3-hour window every day. Missing that window reduces effectiveness quickly.
Do birth control pills increase cancer risk?
They slightly increase the risk of breast and cervical cancer while you’re taking them, but the risk goes back to normal after you stop. At the same time, they significantly reduce your risk of ovarian, endometrial, and colon cancer. For most women, the long-term protective benefits outweigh the small, temporary increases in risk. Talk to your doctor if you have a family history of these cancers.




matthew dendle
December 12, 2025 AT 09:04Jimmy Kärnfeldt
December 13, 2025 AT 17:07Paul Dixon
December 15, 2025 AT 09:43Aidan Stacey
December 17, 2025 AT 06:30Mia Kingsley
December 18, 2025 AT 10:37Jean Claude de La Ronde
December 20, 2025 AT 01:59Katherine Liu-Bevan
December 20, 2025 AT 11:09Monica Evan
December 21, 2025 AT 08:33Eddie Bennett
December 22, 2025 AT 21:14Jim Irish
December 23, 2025 AT 22:18Ariel Nichole
December 24, 2025 AT 09:21Sylvia Frenzel
December 25, 2025 AT 07:22Vivian Amadi
December 25, 2025 AT 13:25