Warfarin-NSAID Risk Calculator
Assess Your Risk
Enter your NSAID choice and usage pattern to calculate your bleeding risk.
Your Risk Assessment
When you're on warfarin to prevent dangerous blood clots, even a simple over-the-counter painkiller can put you in the hospital. This isn't a hypothetical risk - it's a well-documented, life-threatening interaction that affects millions of people every year. The combination of warfarin and NSAIDs doesn't just raise the chance of bleeding - it doubles it. And most people have no idea.
How Warfarin Works - And Why NSAIDs Are So Dangerous
Warfarin has been around since the 1950s, and it works by blocking vitamin K, which your body needs to make clotting factors. Without enough of these factors, your blood takes longer to clot - that’s the whole point. But it’s a tight balance. Too little, and you risk clots. Too much, and you bleed.
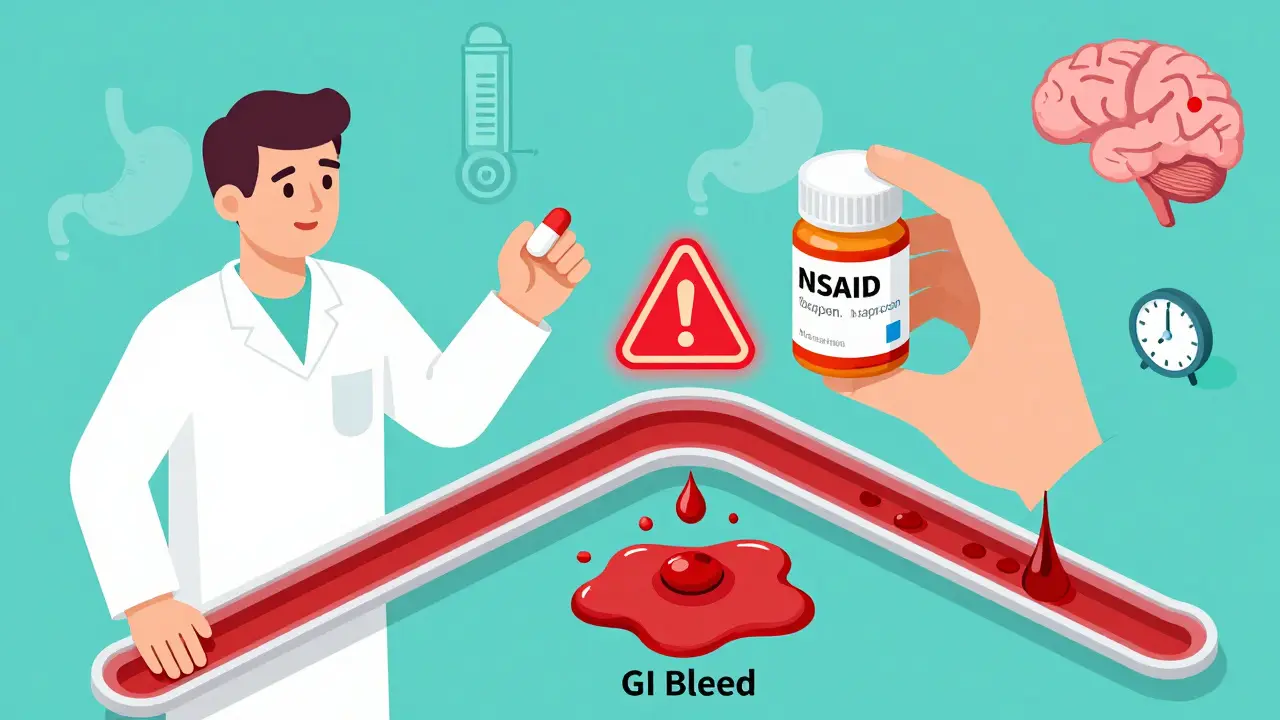
NSAIDs - like ibuprofen, naproxen, diclofenac, and even meloxicam - don’t just reduce pain and swelling. They also mess with your platelets. These tiny blood cells are your body’s first responders when you get a cut. NSAIDs stop them from sticking together properly. That’s why they’re used for heart attacks and strokes - but when you’re already on warfarin, this effect becomes a disaster.
It’s not just one problem. It’s two. Warfarin slows clotting. NSAIDs stop platelets from working. Together, they create a perfect storm. Studies show this combo increases major bleeding risk by more than twice. That’s not a small uptick. That’s a medical emergency waiting to happen.
Which NSAIDs Are the Worst?
Not all NSAIDs are created equal when it comes to bleeding risk. Naproxen is the most dangerous. People taking naproxen with warfarin have over four times the risk of bleeding compared to warfarin alone. Diclofenac isn’t far behind - around 3.3 times higher. Ibuprofen? Better, but still risky - 1.79 times higher. And meloxicam? Surprisingly high risk, even though it’s often labeled as "gentler."
Here’s the myth that gets people killed: "COX-2 inhibitors like celecoxib are safer." That’s not true. Multiple studies, including a 2020 meta-analysis, show they carry the same bleeding risk as traditional NSAIDs when taken with warfarin. Your stomach lining still gets damaged. Your platelets still get disabled. The risk doesn’t go away.
Where the Bleeding Happens - And How Bad It Gets
Bleeding from this combo doesn’t just mean a bloody nose. It’s often internal, silent, and deadly. The most common site? The gut. Gastrointestinal bleeding jumps 2.24-fold. That’s why so many people end up in the ER with black, tarry stools or vomiting blood. But it doesn’t stop there.
Brain bleeds? Risk goes up 3.22 times. Lung bleeds? Up 1.36 times. Urinary tract bleeding? 1.57 times higher. And here’s the scary part - many of these bleeds happen without warning. One patient reported their hemoglobin dropped from 14 to 8 g/dL in just 24 hours after taking ibuprofen for a headache. That’s a blood transfusion-level emergency.
According to the FDA’s Adverse Event Reporting System, over 1,800 bleeding events linked to warfarin-NSAID use were reported between 2015 and 2020. Over 60% of those were GI bleeds. And 78% of people who bled while on this combo ended up hospitalized - for an average of more than five days.

Why People Keep Taking NSAIDs Anyway
You’d think doctors would just say "no." But the reality is messier. Many patients don’t tell their doctor they’re taking ibuprofen for arthritis pain or naproxen for backaches. Over-the-counter means "harmless" in their minds. A 2021 study found that in 68% of warfarin-related bleeding cases, the patient hadn’t disclosed NSAID use.
Doctors aren’t always warned either. In over 40% of U.S. hospitals, electronic health record systems don’t flag this interaction. So even if the patient says "I take Advil," the system might not scream "DANGER."
And then there’s the myth that "newer blood thinners" like apixaban or rivaroxaban are safe with NSAIDs. Not true. A 2019 study in Circulation showed NSAIDs still raise bleeding risk with NOACs - just maybe not as high as with warfarin. But that’s not a green light. It’s still risky.
What to Do Instead - Real Alternatives
If you’re on warfarin and need pain relief, acetaminophen (Tylenol) is your safest bet. It doesn’t touch platelets or clotting factors. It’s not perfect - too much can hurt your liver - but for short-term pain, it’s the best choice.
Topical options work too. Capsaicin creams, lidocaine patches, or even menthol gels can ease joint or muscle pain without affecting your blood. They’re not strong for severe pain, but for mild to moderate, they’re a game-changer.
Physical therapy, heat packs, or even acupuncture can reduce reliance on pills. One 2023 study found that warfarin patients who used physical therapy for osteoarthritis cut their NSAID use by 60% over six months.
What If You Absolutely Must Take an NSAID?
Some doctors may say "go ahead, but be careful." If that’s your situation - and you’ve been advised to do it - here’s what you need to do:
- Use the lowest possible dose - no more than 3-5 days.
- Avoid naproxen, diclofenac, and meloxicam. If you must, ibuprofen is the least risky.
- Get your INR checked before you start, then again 3-5 days after.
- Check it weekly while you’re taking it - even if you feel fine.
- Take a proton pump inhibitor (like omeprazole) to protect your stomach.
- Know the signs of bleeding: dark stools, unusual bruising, blood in urine, dizziness, severe headaches.
And never, ever start an NSAID without telling your anticoagulation clinic or pharmacist. This isn’t something to wing.
The Bigger Picture - Why This Keeps Happening
There are 3.1 million Americans on warfarin. Seventeen million use NSAIDs every month. Millions of them are doing this combo. The cost? Over $1.8 billion a year in hospital bills.
And despite decades of warnings, 42% of warfarin patients still get NSAID prescriptions every year. Why? Because it’s invisible. You don’t feel the risk until you’re bleeding. Because patients don’t think OTC means dangerous. Because doctors are busy. Because systems don’t alert them.
There’s a shift happening. Between 2015 and 2022, warfarin-NSAID co-prescribing dropped 27%. But here’s the twist: NSAID use with newer anticoagulants went up 35%. People think, "I switched to Eliquis, so I can take ibuprofen now." That’s a dangerous assumption. The risk is still there.
Final Rule: Don’t Guess. Ask.
If you’re on any blood thinner - warfarin, apixaban, rivaroxaban, dabigatran - and you’re thinking about taking an NSAID, stop. Don’t take it. Don’t assume it’s safe. Don’t rely on a label that says "for pain."
Ask your pharmacist. Ask your doctor. Ask your anticoagulation clinic. They’ve seen this before. They know what happens. And they’ll tell you: skip the NSAID. Use acetaminophen. Try a patch. Go to physical therapy. Do something else.
This isn’t about being careful. It’s about survival. One pill. One decision. Could save your life.
Can I take ibuprofen with warfarin if I only use it once in a while?
Even occasional use of ibuprofen with warfarin increases your bleeding risk by nearly 80%. A single dose can trigger a drop in platelet function and raise your INR. If you must use it, get your INR checked 3-5 days after taking it. But the safest answer is no - use acetaminophen instead.
Are COX-2 inhibitors like celecoxib safer than regular NSAIDs when on warfarin?
No. Studies show celecoxib and other COX-2 inhibitors carry the same bleeding risk as naproxen or ibuprofen when combined with warfarin. They still damage the stomach lining and interfere with platelet function. The idea that they’re safer is a myth that has cost lives.
What should I do if I accidentally took an NSAID while on warfarin?
Call your anticoagulation clinic or pharmacist immediately. Don’t wait for symptoms. Get your INR checked within 3 days. Watch for signs of bleeding: unusual bruising, dark stools, blood in urine, dizziness, or severe headaches. If you feel weak or lightheaded, go to the ER. Don’t assume you’re fine just because you only took one pill.
Why do some doctors still prescribe NSAIDs with warfarin?
Some doctors may believe short-term use is safe, especially for patients with severe arthritis. But major guidelines from the American College of Cardiology and American Heart Association clearly state NSAIDs should be avoided. This practice persists due to outdated beliefs, lack of awareness, or pressure from patients who don’t understand the risk.
Do newer blood thinners like Eliquis or Xarelto avoid this risk?
No. While newer anticoagulants (NOACs) have fewer drug interactions overall, NSAIDs still increase bleeding risk with them. Studies show a 2-3 times higher risk of GI bleeding with NSAIDs on apixaban or rivaroxaban. The risk is lower than with warfarin, but it’s still real. Never assume a newer drug makes NSAIDs safe.