When you need a nerve block, the choice of anesthetic matters. Not all local anesthetics are built the same. Prilocaine stands out for its safety profile, especially when you’re looking for a reliable option with fewer side effects. Unlike lidocaine or bupivacaine, prilocaine doesn’t carry the same risk of serious heart or nerve toxicity at standard doses. That’s why it’s increasingly used in dental procedures, IV regional anesthesia, and even minor surgical nerve blocks where precision and safety are key.
How Prilocaine Works in Nerve Blocks
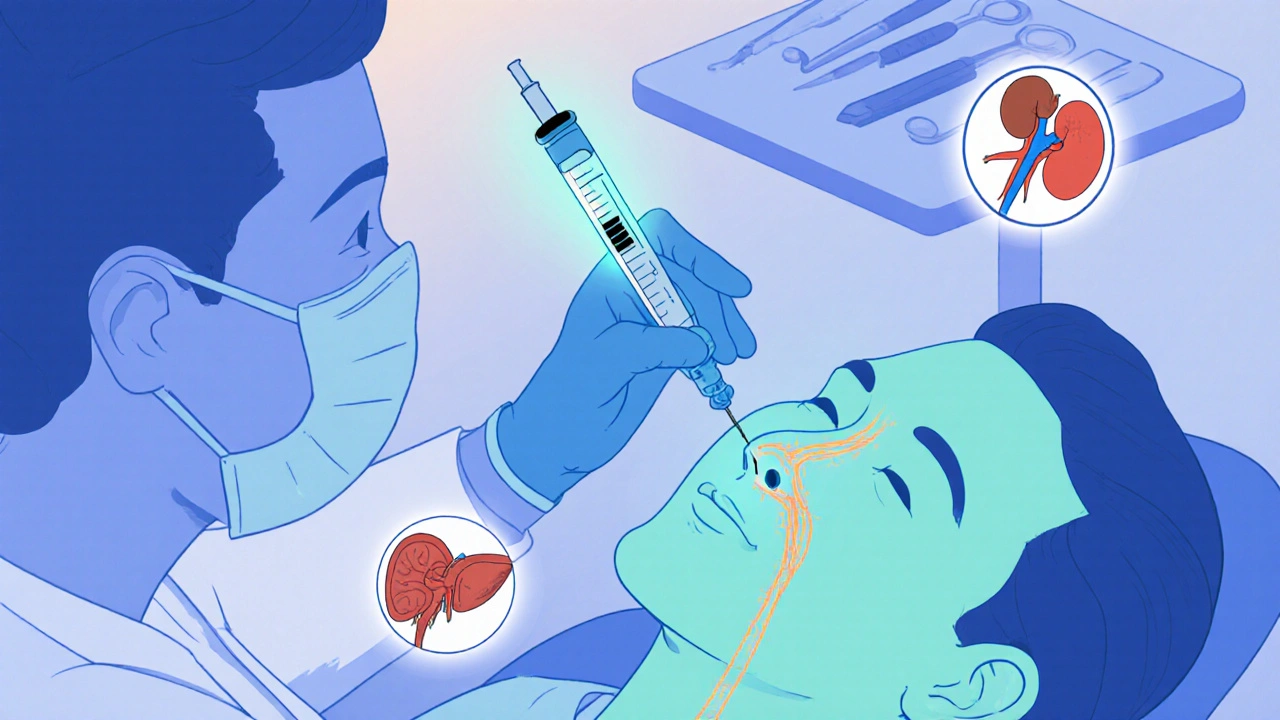
Prilocaine blocks sodium channels in nerve cells, stopping pain signals before they reach your brain. It starts working in about 5 to 10 minutes and lasts between 1 to 2 hours-long enough for most minor procedures but short enough to reduce lingering numbness. What makes it different is how quickly your body breaks it down. Prilocaine is metabolized in the liver and kidneys, and its main byproduct, ortho-toluidine, is less likely to cause methemoglobinemia than other anesthetics when used correctly.
It’s often mixed with epinephrine to prolong its effect and reduce bleeding at the injection site. In dental nerve blocks, for example, a 3% solution of prilocaine with epinephrine gives patients solid numbness without the jittery side effects you sometimes get with higher doses of lidocaine.
Why Prilocaine Is Safer for Many Patients
One of the biggest advantages of prilocaine is its lower toxicity. Studies from the Journal of Clinical Anesthesia show that prilocaine has a higher therapeutic index than lidocaine-meaning there’s a wider gap between the effective dose and the toxic dose. That’s critical in situations where you can’t precisely control how much anesthetic enters the bloodstream, like in finger blocks or when multiple injections are needed.
Patients with liver disease, older adults, or those on multiple medications often tolerate prilocaine better. It doesn’t interact badly with common heart medications like beta-blockers, and it doesn’t cause the same level of vasodilation that can lead to rapid absorption and overdose. In fact, the FDA has approved prilocaine for use in pregnant women for dental procedures, a category where many other anesthetics are used with caution.
Lower Risk of Methemoglobinemia-But It’s Still Possible
Prilocaine’s biggest drawback is its potential to cause methemoglobinemia, a rare condition where red blood cells can’t carry oxygen properly. But here’s the key: it only happens with high doses or repeated use. A single nerve block using standard doses (under 400 mg in adults) carries almost no risk. The real danger comes from using prilocaine cream for large areas of skin-like in laser hair removal or tattoo removal-where hundreds of milligrams can be absorbed.
For nerve blocks, you’re typically using 10 to 50 mg per injection. At that level, methemoglobinemia is extremely rare. Clinics that use prilocaine for pediatric nerve blocks or in patients with a history of anemia still prefer it over alternatives because the benefit outweighs the risk when dosed properly.

Prilocaine vs. Other Local Anesthetics
Comparing prilocaine to other options helps explain why it’s chosen in specific cases:
| Anesthetic | Onset Time | Duration | Toxicity Risk | Methemoglobinemia Risk |
|---|---|---|---|---|
| Prilocaine | 5-10 min | 1-2 hours | Low | Very low (at standard doses) |
| Lidocaine | 2-5 min | 1-2 hours | Medium | None |
| Bupivacaine | 10-20 min | 4-8 hours | High | None |
| Ropivacaine | 10-15 min | 3-6 hours | Medium | None |
Prilocaine doesn’t last as long as bupivacaine, so it’s not ideal for major surgeries. But for outpatient procedures-like removing a cyst, repairing a finger laceration, or dental work-it’s often the best middle ground. It’s faster than ropivacaine and safer than lidocaine for patients with heart conditions.
Real-World Use Cases
Prilocaine is the go-to anesthetic in many emergency departments for hand and finger blocks. Why? Because you can inject it near the wrist or base of the finger without worrying about accidental intravascular injection. If you hit a small artery, the risk of systemic toxicity is much lower than with lidocaine.
In dentistry, 3% prilocaine with 1:200,000 epinephrine is the standard for inferior alveolar nerve blocks. It gives complete numbness of the lower jaw and teeth without the prolonged numbness or tingling that some patients report with lidocaine. Parents of young children often prefer it because kids wake up faster and don’t chew their lips or tongue afterward.
Even in outpatient plastic surgery, prilocaine is used for tumescent anesthesia in minor liposuction or skin grafts. Its low tissue irritation and minimal systemic absorption make it ideal for areas with lots of small blood vessels.
Who Should Avoid Prilocaine?
Prilocaine isn’t for everyone. You should avoid it if you’ve had a previous allergic reaction to amide-type anesthetics (though true allergies are rare). Also, people with severe G6PD deficiency-where red blood cells break down too easily-should be cautious, as prilocaine can trigger hemolysis in these cases.
Patients on nitroglycerin or other nitrates should also be monitored. The combination can increase the risk of low blood pressure, especially if epinephrine is added. And while prilocaine is generally safe in pregnancy, it’s still best to use the lowest effective dose.
How to Maximize Safety During Use
Here’s what works in real clinical practice:
- Always aspirate before injecting-pull back on the syringe plunger to check for blood. This avoids accidental IV injection.
- Use the smallest effective dose. For most nerve blocks, 20-50 mg is enough.
- Never exceed 400 mg total in a single session for an adult.
- Watch for signs of methemoglobinemia: blue-tinged skin, shortness of breath, headache, confusion. If seen, treat with methylene blue immediately.
- For children, weight-based dosing is critical. Use 4 mg/kg as the maximum safe dose.
Most providers who use prilocaine regularly say the same thing: it’s predictable. You know what you’re getting. No surprises. No sudden drops in blood pressure. No prolonged numbness that lasts all day.
What’s the Future for Prilocaine?
Even with newer anesthetics like levobupivacaine and articaine gaining ground, prilocaine hasn’t been replaced. It’s still listed in the WHO Model List of Essential Medicines. That’s because it fills a unique niche: safe, effective, affordable, and easy to store.
Research is now looking at combining prilocaine with newer adjuvants like dexmedetomidine to extend its duration without increasing toxicity. Early trials show promise for longer-lasting nerve blocks in chronic pain management, especially for patients who can’t tolerate opioids.
For now, if you need a nerve block and safety is your top concern-whether you’re a patient or a provider-prilocaine remains one of the most reliable choices on the shelf.
Is prilocaine better than lidocaine for nerve blocks?
Prilocaine is often safer than lidocaine, especially for patients with heart conditions or those needing multiple injections. It has a lower risk of toxicity and doesn’t cause the same level of vasodilation, which means slower absorption into the bloodstream. However, lidocaine works faster and is more widely available. For most routine nerve blocks, prilocaine is preferred when safety is prioritized over speed.
Can prilocaine cause nerve damage?
Prilocaine itself doesn’t damage nerves. Like all local anesthetics, nerve injury from a nerve block is almost always due to the needle or injection pressure-not the drug. Proper technique, avoiding direct injection into a nerve, and using ultrasound guidance when possible reduce this risk significantly. Prilocaine is no more likely to cause nerve damage than lidocaine or bupivacaine.
How long does prilocaine last in a nerve block?
Prilocaine typically lasts 1 to 2 hours when used alone, and up to 3 hours when mixed with epinephrine. This makes it ideal for short procedures like dental work, minor skin surgeries, or finger repairs. It doesn’t last as long as bupivacaine, so it’s not used for post-op pain lasting more than a few hours.
Is prilocaine safe during pregnancy?
Yes, prilocaine is considered safe for use in pregnant women, especially for dental procedures. The FDA classifies it as Category B, meaning animal studies show no risk and human data supports its safety in low doses. As with any medication, use the lowest effective dose and avoid unnecessary injections.
What are the signs of prilocaine overdose?
Signs include ringing in the ears, metallic taste, dizziness, muscle twitching, seizures, and low blood pressure. In rare cases, it can cause methemoglobinemia, which shows up as bluish skin or lips and trouble breathing. If you suspect an overdose, stop the injection immediately and seek medical help. Treatment may include oxygen, IV fluids, or methylene blue for methemoglobinemia.
If you’re scheduled for a procedure involving a nerve block, ask your provider if prilocaine is an option. For many people, it’s the quiet hero of local anesthesia-less flashy than the alternatives, but far more dependable when it counts.

kim pu
November 18, 2025 AT 21:33Prilocaine? LOL. They say it's 'safe' but did you know Big Pharma quietly phased out the 4% version because it was turning patients blue? Methemoglobinemia isn't 'rare'-it's covered up. I know a nurse who lost a patient after a 'routine' dental block. They called it 'idiosyncratic reaction.' Bullshit. They don't want you to know.
benedict nwokedi
November 19, 2025 AT 15:20Oh, so now we're trusting FDA approvals? Please. The same agency that greenlit Vioxx and OxyContin is now telling us prilocaine is 'safe'? The therapeutic index is a statistical illusion-real people don't live in bell curves. And epinephrine? That's just adrenaline with a fancy name. You think your 'low-dose' injection isn't flooding your system? Wake up.
deepak kumar
November 21, 2025 AT 02:36As a dentist in Mumbai, I use prilocaine daily-3% with epinephrine, no issues. Kids smile after procedures, no lip-biting. My senior taught me: 'It's not the drug, it's the dose.' Prilocaine is quiet, reliable, like a good chai-no hype, just works. And yes, aspirate. Always. 😊
Dave Pritchard
November 22, 2025 AT 19:56Just want to say thanks for this detailed breakdown. I'm a new PA and I was nervous about using prilocaine after reading scary Reddit threads. This helped me understand the real risk profile. It's not perfect, but for outpatient stuff? Yeah, it's a solid tool. Always start low, watch for signs, and don't panic. You got this.
malik recoba
November 24, 2025 AT 14:52i read this whole thing and i think prilocaine is cool? like, i dont know much about meds but i trust my dentist uses it and my fingers dont turn blue so… maybe it’s fine? i just want to not feel pain lol
Sarbjit Singh
November 26, 2025 AT 02:28Prilocaine is the unsung hero of local anesthesia 😊 I’ve used it in rural clinics where we don’t have ultrasound or fancy monitors. Simple, cheap, works. Just don’t give more than 50 mg per injection. And yes, aspirate! 🙏
Angela J
November 26, 2025 AT 22:47Okay but… what if they’re secretly using prilocaine to test how many people develop methemoglobinemia? I mean, why is it the only one that causes this? And why is it still on the WHO list? Coincidence? Or… are they tracking who gets sick? I’ve seen people get ‘flu-like symptoms’ after dental work… they never connect the dots.
Sameer Tawde
November 27, 2025 AT 12:05Prilocaine = perfect for minor blocks. Fast enough, safe enough, cheap enough. No drama. Just do your job right. Aspirate. Dose right. Done. 💪
Erica Lundy
November 28, 2025 AT 09:44The epistemological foundation of clinical preference rests not upon pharmacological superiority, but upon the cultural codification of safety within institutional memory. Prilocaine, as a molecule, is neutral; its valorization emerges from the epistemic authority of peer-reviewed journals and the bureaucratic inertia of formularies. To call it 'reliable' is to mistake convention for certainty.
Kevin Jones
November 28, 2025 AT 14:34Prilocaine isn't just an anesthetic-it's a *statement*. In a world of overmedicated, overhyped, overpriced pharma solutions, prilocaine whispers: 'I don't need to be flashy to be effective.' It's the anti-vibes anesthetic. The quiet rebel. The unsung hero. And yes, I cried when I saw that table comparing toxicity levels.
Premanka Goswami
November 29, 2025 AT 11:55They say prilocaine is safe… but who funded the studies? Who owns the patents? The same conglomerate that sells your antidepressants and your 5G towers. They want you numb, but not too numb-just enough to stay compliant. Methemoglobinemia? A feature, not a bug. It keeps the 'high-risk' patients in the system longer. Think about it.
Alexis Paredes Gallego
November 29, 2025 AT 17:35PRILICAINE IS A GOVERNMENT COVER-UP. THEY KNOW LIDOCAINE IS BETTER. BUT THEY PUSHED PRILICAINE BECAUSE IT’S CHEAPER TO MAKE AND IT MAKES PEOPLE QUESTION THE SYSTEM. WHEN YOU ASK WHY IT’S ‘SAFER,’ THEY SAY ‘THERAPEUTIC INDEX’-BUT THAT’S JUST A WORD TO MAKE YOU FEEL SAFE WHILE THEY EXPERIMENT ON YOU. I’VE SEEN THE DOCUMENTS. THEY’RE HIDDEN IN THE NIH ARCHIVES. ASK FOR FOIA. I DARE YOU.
Saket Sharma
December 1, 2025 AT 10:34Prilocaine’s 'low toxicity' is a myth peddled by industry-funded journals. Bupivacaine has higher cardiac risk? So what? You’re not injecting it into a vein. Proper technique negates all risks. Prilocaine’s real flaw? It’s too easy. No prestige. No drama. No billing code for 'complication management.' It’s a tool for the lazy clinician.
Shravan Jain
December 1, 2025 AT 22:55Prilocaine: 10-50mg per block. But how many patients get 2-3 blocks in one visit? How many are on multiple meds? How many have undiagnosed G6PD? The data is aggregated. The outliers are ignored. The system rewards volume, not vigilance. This post reads like a pharma pamphlet. Where's the real risk analysis? Where's the harm?
Brandon Lowi
December 3, 2025 AT 22:44Prilocaine? That’s a socialist anesthetic. No flair. No patriotism. No American-made innovation. Lidocaine? Made here. Tested here. Trusted here. Prilocaine? Made in some overseas lab with a 3-star FDA rating. We’re outsourcing our pain relief while they export our health risks. Wake up, America. Use what’s ours.