SGLT2 Inhibitors and Kidney Function: What You Need to Know
When you hear SGLT2 inhibitors, a class of oral diabetes medications that lower blood sugar by making the kidneys remove excess glucose through urine. Also known as sodium-glucose cotransporter 2 inhibitors, these drugs don’t just control blood sugar—they’re now recognized for their ability to slow kidney damage in people with type 2 diabetes and chronic kidney disease. That’s not a side effect. It’s the point.
Unlike older diabetes meds that force the body to produce more insulin or make cells more sensitive to it, SGLT2 inhibitors work directly in the kidneys. They block a protein called SGLT2, which normally reabsorbs sugar from the urine back into the bloodstream. When that protein is blocked, sugar leaves the body through pee. That lowers blood sugar naturally—and it also reduces pressure inside the kidneys. High pressure is one of the main reasons kidneys fail in diabetics. By lowering that pressure, these drugs help the kidneys last longer. Studies like the CREDENCE trial showed that canagliflozin reduced the risk of kidney failure, dialysis, or death from kidney disease by over 30% in high-risk patients. Empagliflozin and dapagliflozin showed similar results in other large trials. This isn’t theoretical. It’s real, measurable protection.
These drugs also help with heart failure, fluid retention, and high blood pressure—all conditions that often go hand-in-hand with kidney disease. That’s why doctors now prescribe them not just for blood sugar control, but for overall organ protection. You don’t need to have advanced kidney disease to benefit. Even early-stage kidney damage can be slowed. And if you’re on insulin or other diabetes meds, SGLT2 inhibitors can often be added safely without causing low blood sugar. They’re not for everyone—people with severe kidney impairment, recurrent urinary infections, or certain dehydration risks need to be careful—but for millions, they’ve become a cornerstone of long-term health.
What you’ll find below are posts that dig into how these drugs fit into real-world care. You’ll see how they compare to other diabetes treatments, what side effects to watch for, how they interact with common medications, and why some patients do better than others. There’s no fluff. Just clear, practical info from people who’ve seen how these drugs change lives—and kidneys—for the better.
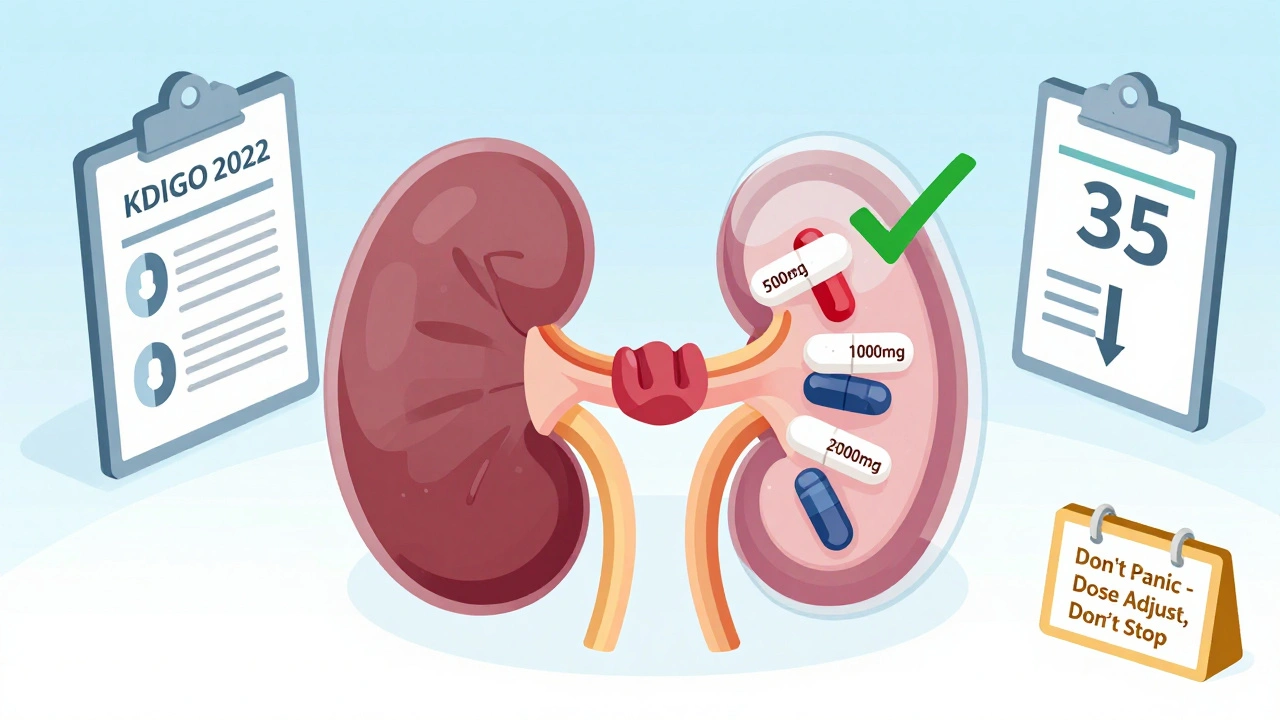
Updated 2025 guidelines for metformin and SGLT2 inhibitor dosing in kidney disease. Learn when to adjust doses, when to stop, and how to navigate conflicting FDA labels and clinical evidence.
View More