Renal Dosing Calculator for Metformin and SGLT2 Inhibitors
Enter the patient's eGFR value (mL/min/1.73 m²)
When managing type 2 diabetes in patients with chronic kidney disease, getting the dosing right isn’t just about blood sugar-it’s about protecting the kidneys and avoiding life-threatening side effects. The rules for metformin and SGLT2 inhibitors have changed dramatically in the last five years, and many clinicians are still adjusting. If you’re prescribing these drugs and your patient’s eGFR is falling, you’re not alone in wondering: When do I hold the drug? When do I keep going?
Metformin: The Old Rules Are Out
For years, metformin was pulled at the first sign of kidney trouble. If eGFR dropped below 60 mL/min/1.73 m², you stopped it. That was the rule. But in 2016, the FDA revised its stance after reviewing data from over 100,000 patients. The risk of lactic acidosis? Extremely low-just 3.3 cases per 100,000 patient-years. That’s less than being struck by lightning.
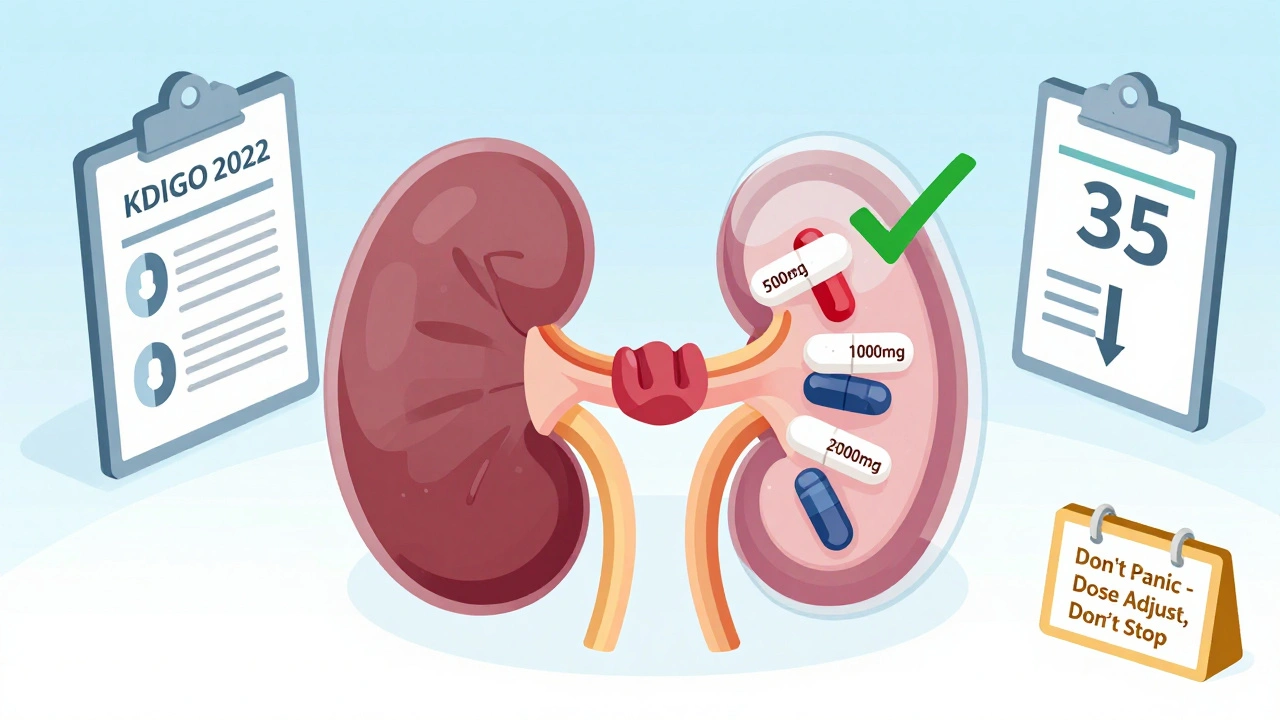
Today, metformin isn’t banned at eGFR 45-59. You can still use it, but you cut the dose. Maximum daily dose drops from 2550 mg to 2000 mg. At eGFR 30-44, you’re capped at 1000 mg per day. And yes, you can still use it-even at eGFR 20-29-if the patient is stable, well-hydrated, and has no other risk factors like heart failure or sepsis. Some experts quietly prescribe 500 mg daily in stable patients with eGFR as low as 15, though that’s off-label and requires close monitoring.
The key is not to panic at every small drop in eGFR. Metformin doesn’t cause kidney damage. It’s the other way around-kidneys failing make it harder to clear the drug. So if your patient’s eGFR falls from 48 to 42, don’t pull metformin. Just reduce the dose and check again in 3 months.
SGLT2 Inhibitors: The Game Changers
SGLT2 inhibitors-drugs like dapagliflozin, empagliflozin, and canagliflozin-were originally approved only for blood sugar control. But then came the trials: CREDENCE, DAPA-CKD, EMPA-KIDNEY. They showed something shocking: these drugs don’t just lower glucose. They slow kidney failure, reduce heart attacks, and cut death rates by 30-40% in people with chronic kidney disease.
That’s why KDIGO updated its guidelines in 2022. They said: Start an SGLT2 inhibitor if eGFR is 20 or higher. That’s a huge shift. Before, you couldn’t use canagliflozin if eGFR was below 45. Now, you’re encouraged to use it even when kidneys are already damaged.
Here’s the catch: each drug has its own rules.
- Canagliflozin: Max 100 mg/day if eGFR is 45-59. Don’t use if eGFR is below 45.
- Dapagliflozin: Max 10 mg/day if eGFR is 25-45. Contraindicated below 25.
- Empagliflozin: Max 10 mg/day if eGFR is 30-45. Don’t use below 30.
But here’s the twist: once you start an SGLT2 inhibitor, you can often keep it going-even if eGFR drops below the labeled threshold. The initial dip in eGFR (usually 2-5 mL/min/1.73 m²) is normal. It’s not kidney damage. It’s the drug doing its job-reducing pressure in the glomeruli to protect the filters. Many patients’ eGFR rebounds after 3 months. If you stop the drug because of that dip, you’re robbing them of long-term kidney protection.
The Overlap Zone: eGFR 20-29
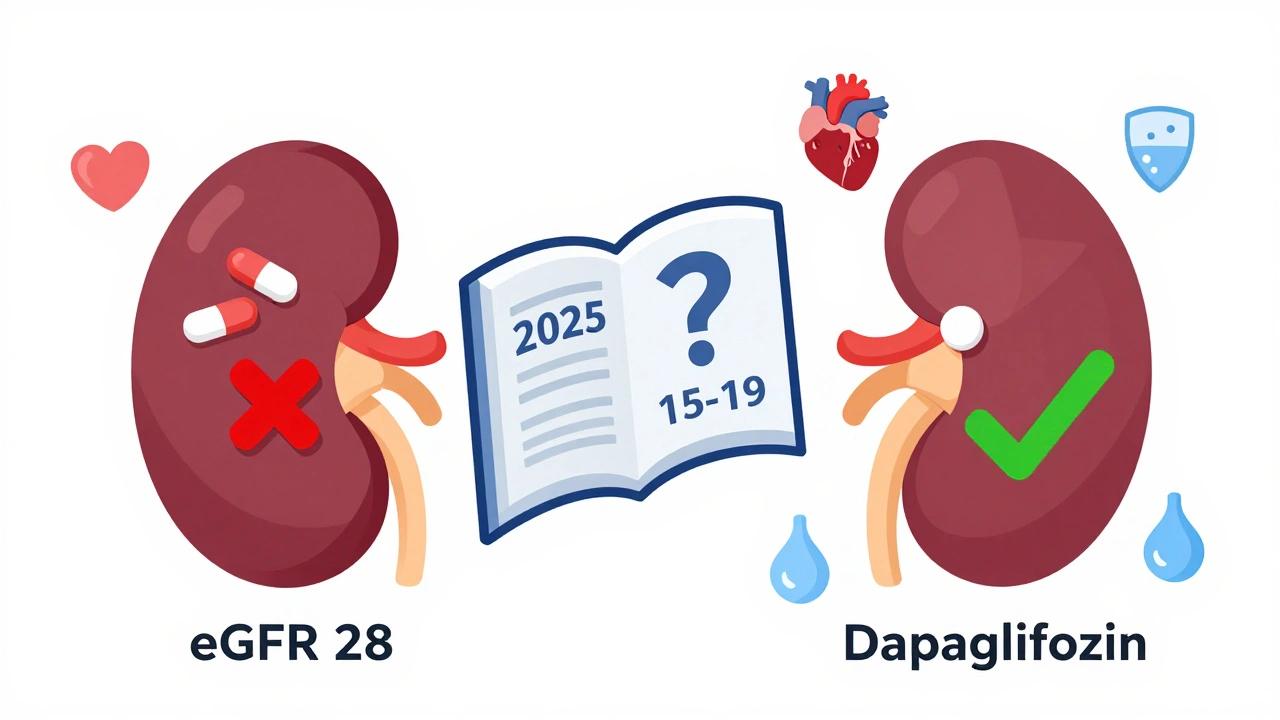
This is the trickiest area. You can use an SGLT2 inhibitor here-KDIGO says yes. But metformin? You’re supposed to stop it. The guidelines say: discontinue metformin if eGFR falls below 30. So if your patient has eGFR 25, you can keep dapagliflozin but must stop metformin.
That’s a problem for many patients. Metformin is cheap, effective, and reduces cardiovascular death. Pulling it leaves a gap. Some clinicians will keep metformin at 500 mg in this range if the patient is stable, well-hydrated, and has no other risk factors. But that’s not guideline-aligned. Insurance won’t cover it. And if something goes wrong, you’re on shaky ground.
The safest path: switch from metformin to an SGLT2 inhibitor when eGFR drops below 30. Don’t combine them in the 20-29 range. Use the SGLT2 inhibitor as your primary glucose-lowering agent here. It’s doing more than just lowering sugar-it’s protecting the kidneys.
Monitoring: What to Check and When
Monitoring isn’t optional. It’s the difference between safe use and disaster.
- Metformin: Check eGFR every 6-12 months if it’s above 60. Every 3-6 months if it’s 45-59. Every 3 months if it’s 30-44.
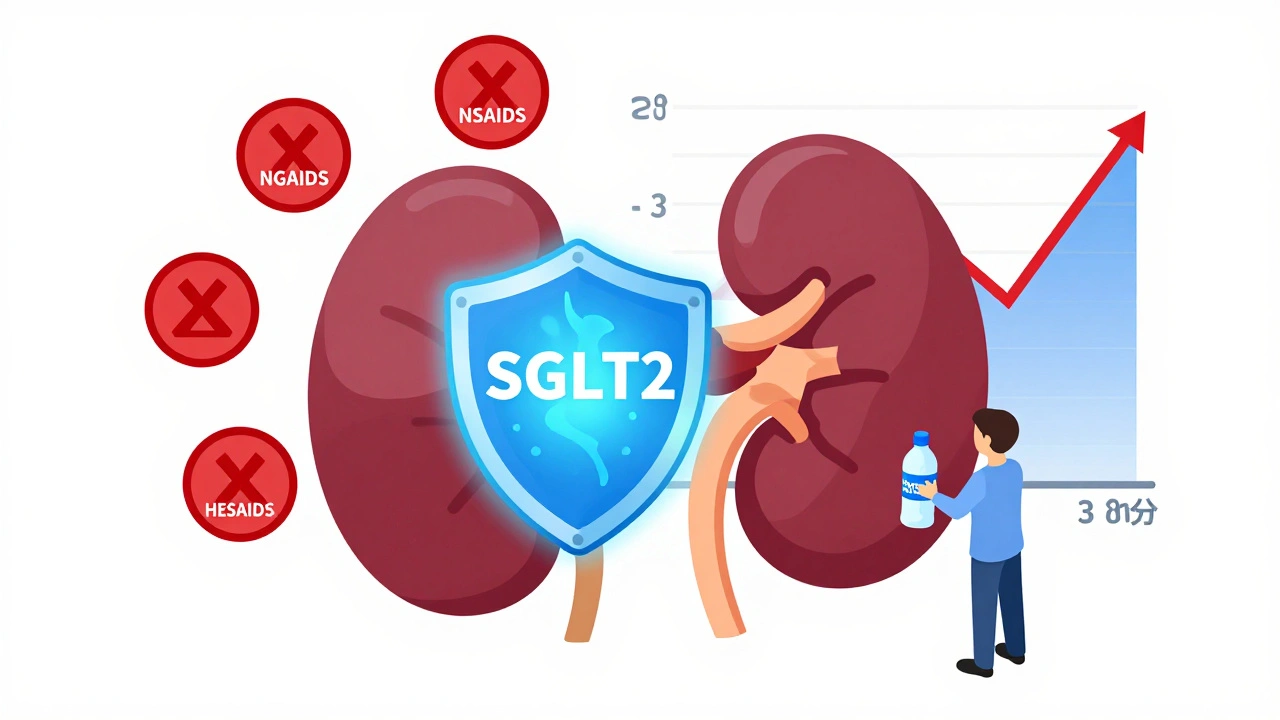
- SGLT2 inhibitors: Check eGFR within 4 weeks of starting. Then every 3 months. Watch for a drop-but don’t panic. If it falls 5-10% and stabilizes, keep going. If it keeps falling fast, look for other causes: dehydration, NSAID use, heart failure.
Also, watch for volume depletion. These drugs make you pee more. If your patient is on a loop diuretic, or has poor oral intake, or is sick with the flu, they’re at higher risk for acute kidney injury. Teach them “sick-day rules”: stop the SGLT2 inhibitor if they’re vomiting, not eating, or dehydrated. Restart only when they’re back to normal.
Regulatory vs. Clinical Reality
Here’s where things get messy. The FDA still says canagliflozin is contraindicated below eGFR 45. Dapagliflozin’s label says don’t use below 25. But KDIGO and ADA say: use them down to 20. And the evidence is strong.
Many clinicians face pressure from insurance companies. A 2022 survey found 43% of endocrinologists had claims denied for SGLT2 inhibitors in patients with eGFR 20-29. You have to fight. Write appeals. Cite KDIGO 2022. Attach the trial data. Some payers are starting to catch up.
Some hospitals now have protocols that allow SGLT2 inhibitors below FDA thresholds if nephrology signs off. That’s the new standard. If your hospital doesn’t have one, push for it.
What About Dialysis?
There’s no clear guidance here. Metformin is generally avoided on dialysis because it’s cleared by the kidneys-but peritoneal dialysis patients can sometimes take 250 mg daily. Hemodialysis patients might get 500 mg after the session. But data is thin. Most experts avoid it entirely on dialysis.
SGLT2 inhibitors? Not approved for use on dialysis. The trials didn’t include patients on dialysis. Don’t use them. The benefit hasn’t been proven, and the risk of volume depletion is higher.
What’s Coming Next?
The FDA approved dapagliflozin for chronic kidney disease in 2024-even in people without diabetes. That’s huge. It means these drugs are now seen as kidney protectors first, diabetes drugs second.
ADA and KDIGO are working on a 2025 update. Early drafts are looking at whether SGLT2 inhibitors can be used safely in patients with eGFR 15-19. That’s the next frontier.
For now, the message is clear: don’t underuse these drugs because of outdated rules. If your patient has type 2 diabetes and CKD, and eGFR is 20 or higher, an SGLT2 inhibitor should be part of the plan. If metformin is still going, keep it-but adjust the dose. If eGFR drops below 30, switch to the SGLT2 inhibitor and stop metformin.
The goal isn’t just to control glucose. It’s to keep patients off dialysis. To keep them alive longer. And the evidence says these drugs do that better than anything else we’ve had in nephrology for decades.
Can I keep metformin if my patient’s eGFR is 28?
No. According to ADA and KDIGO guidelines, metformin should be discontinued when eGFR falls below 30 mL/min/1.73 m². At eGFR 28, the risk of lactic acidosis increases, even if the patient seems stable. Switch to an SGLT2 inhibitor like dapagliflozin, which is still safe and recommended at this level.
Why does eGFR drop after starting an SGLT2 inhibitor?
The drop is usually 2-5 mL/min/1.73 m² and happens in the first 4-6 weeks. It’s not kidney damage-it’s a sign the drug is working. SGLT2 inhibitors reduce pressure in the kidney’s filtering units (glomeruli), which lowers protein leakage and protects long-term function. Most patients’ eGFR stabilizes or even improves after 3 months. Don’t stop the drug unless eGFR keeps falling or symptoms of dehydration appear.
Is it safe to use SGLT2 inhibitors with loop diuretics?
It can be, but you need to be cautious. Both drugs increase urine output. Together, they raise the risk of dehydration and acute kidney injury, especially in older adults or those with heart failure. Monitor fluid intake, weight, and eGFR closely. Advise patients to drink more fluids and hold the SGLT2 inhibitor during illness or heat exposure. Consider reducing the diuretic dose if possible.
Can I start an SGLT2 inhibitor if the patient has proteinuria but eGFR is 18?
Not according to current guidelines. SGLT2 inhibitors are not recommended below eGFR 20 mL/min/1.73 m². While the drug may still offer benefit, there’s no solid evidence from trials in this range. The risk of volume depletion increases, and the benefit is uncertain. Wait for the 2025 guideline update. For now, focus on ACE inhibitors, SGLT2 inhibitors if eGFR is above 20, and strict blood pressure control.
Why do insurance companies deny SGLT2 inhibitors for eGFR 22?
Because the FDA’s official labeling still says these drugs are contraindicated below higher eGFR thresholds (e.g., 45 for canagliflozin, 25 for dapagliflozin). Insurance systems often rely on FDA labels, not clinical guidelines. To get approval, you need to appeal-cite KDIGO 2022, attach trial summaries, and explain that the drug is being used for kidney protection, not just glucose control. Many insurers are starting to approve these cases, but it still takes effort.

alaa ismail
December 3, 2025 AT 09:12Been prescribing metformin down to eGFR 25 for years with zero lactic acidosis cases. Docs still panic like it's 2010. The data's clear - it's the kidneys failing, not the drug killing them. Just reduce the dose and watch hydration. 🤷♂️
ruiqing Jane
December 5, 2025 AT 03:21Let me just say - if you're still stopping SGLT2 inhibitors at the first 5-point eGFR dip, you're not protecting kidneys. You're protecting your liability portfolio. The drop is a signal, not a stop sign. I've seen patients rebound 15 points after 6 months. Don't be the doctor who kills a life-saving drug because of a lab number.
Paul Santos
December 6, 2025 AT 04:13Ah yes, the classic 'eGFR is a proxy for renal function' fallacy. 🤓 The glomerular pressure hypothesis isn't just elegant - it's *philosophically* profound. SGLT2i don't 'fix' kidneys - they recalibrate the entire hemodynamic paradigm. We're not dosing drugs, we're orchestrating renal symphonies. 🎻
Eddy Kimani
December 6, 2025 AT 04:57Wait - so if dapagliflozin is approved down to eGFR 20, why does the FDA label say 25? Is this a case of guideline drift or regulatory inertia? The evidence is overwhelming, but the systems aren't built for nuance. We're stuck between science and bureaucracy. Anyone else tired of writing appeals?
Saurabh Tiwari
December 6, 2025 AT 11:11Michael Campbell
December 7, 2025 AT 06:28Big Pharma pushed this. They don't care about your patient. They care about selling more pills. That 'kidney protection' is just a marketing gimmick. Metformin's been safe for 50 years - why change now?
Victoria Graci
December 8, 2025 AT 08:03It’s funny how we treat eGFR like a moral compass - drop below 30? You’ve failed. But what if the kidney isn’t failing? What if it’s just… adapting? We’ve turned numbers into narratives, and in doing so, we’ve forgotten the person behind the lab report. Is this medicine - or mathematics with a stethoscope?
Saravanan Sathyanandha
December 10, 2025 AT 04:33In India, we often face a different reality - patients cannot afford newer agents. Metformin remains the backbone. While guidelines are clear, in practice, we carefully continue low-dose metformin (500 mg) in stable CKD stage 4 patients, especially when SGLT2 inhibitors are unaffordable. Close monitoring and patient education are key. We adapt, not just follow.
Fern Marder
December 11, 2025 AT 20:18Y’all are overcomplicating this. If eGFR drops, stop the drug. Period. If they get worse, you get sued. If they stay stable, you get a pat on the back. Don't be the hero. Be the safe one. 💉
Carolyn Woodard
December 12, 2025 AT 21:53Has anyone considered the psychological toll on patients when their meds get pulled at every eGFR dip? They feel like their bodies are failing them - and then you take away the one thing that made them feel in control. Maybe the real issue isn't the drug - it's how we communicate risk. We treat numbers like verdicts, not signals.
Allan maniero
December 14, 2025 AT 15:02I've seen this play out too many times - a patient on metformin with eGFR 32, gets switched to dapagliflozin, eGFR drops to 28, and the PCP panics and stops everything. Then the HbA1c rockets, the patient gains weight, and six months later they're in the ER with DKA. The truth? The real danger isn't metformin at eGFR 28 - it's the fear of doing nothing. We're so scared of being wrong that we end up doing the worst thing: doing nothing at all.
Anthony Breakspear
December 15, 2025 AT 13:52Listen - if you're still telling patients to stop metformin at eGFR 45, you're doing them a disservice. That’s like refusing to give insulin because someone has a cold. The science is settled. The guidelines are updated. The only thing left is your courage to use it. Your patient’s kidneys will thank you. And so will their wallet.
Zoe Bray
December 16, 2025 AT 05:55Per KDIGO 2022 and ADA 2024 guidelines, the use of SGLT2 inhibitors in patients with an eGFR of 20 mL/min/1.73 m² or higher is not merely acceptable - it is strongly recommended for the purpose of slowing progression of chronic kidney disease, irrespective of diabetes status. Discontinuation based on transient eGFR decline constitutes a deviation from evidence-based practice and may compromise long-term clinical outcomes.