Renal Adjustment Metformin: What You Need to Know About Dosing and Safety
When you take metformin, a first-line oral medication for type 2 diabetes that helps lower blood sugar by reducing liver glucose production and improving insulin sensitivity. It's one of the most prescribed drugs in the world—but its safety depends heavily on how well your kidneys are working. If your kidneys aren’t filtering properly, metformin can build up in your body, raising the risk of a rare but serious condition called lactic acidosis. That’s why renal adjustment, the process of changing a drug’s dose based on kidney function isn’t optional—it’s essential.
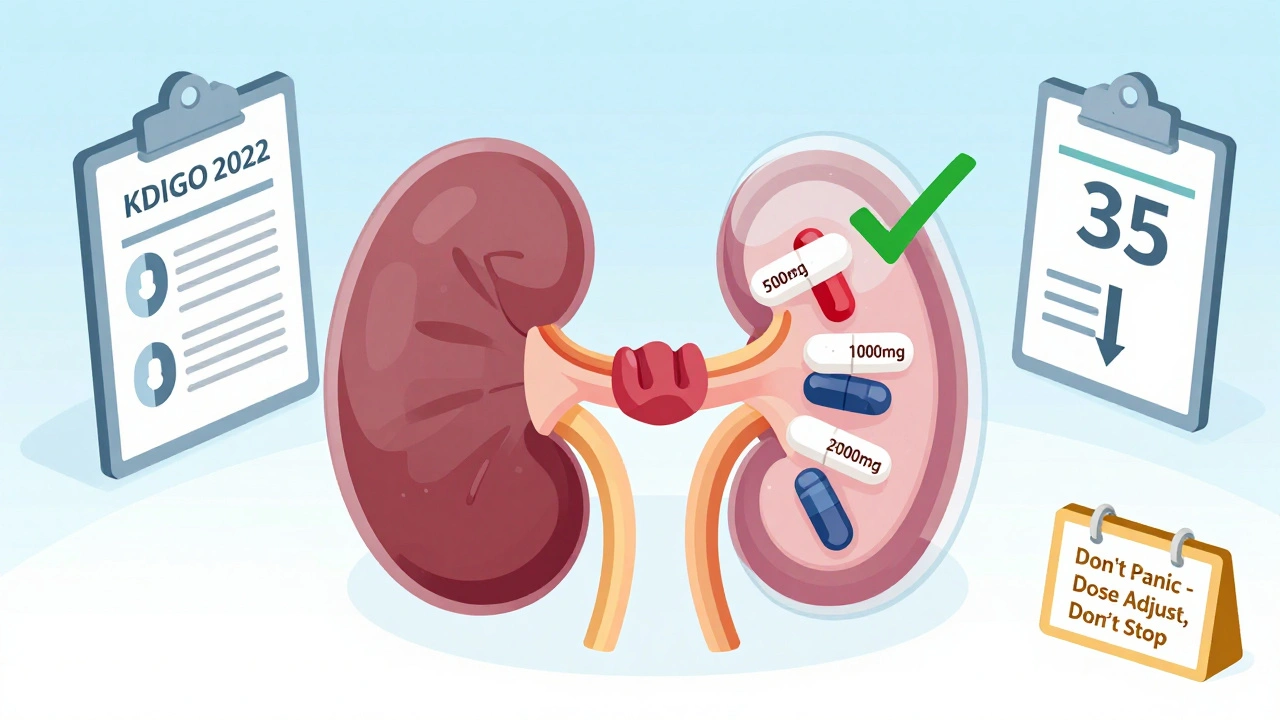
Your kidneys are measured by something called eGFR, estimated glomerular filtration rate, a number that tells you how well your kidneys filter waste from your blood. Doctors use this number to decide if you can keep taking metformin, and if so, how much. If your eGFR is below 30, metformin is usually stopped. Between 30 and 45, the dose is often cut in half. Above 45, most people can stay on standard doses. But it’s not just about the number—age, other medications, and conditions like heart failure also matter. For example, if you’re older and your eGFR is borderline, your doctor might be extra cautious. Some people think if they feel fine, their kidneys must be okay. But kidney damage can sneak up without symptoms until it’s advanced. That’s why regular blood tests are part of managing diabetes long-term.
Metformin doesn’t cause kidney damage, but your kidneys handle it. If your kidney function drops over time, your metformin dose needs to drop too. Many patients don’t realize this until they get a lab result or feel unwell. That’s why checking your eGFR at least once a year—or more often if you’re over 65 or have other health issues—isn’t just a formality. It’s a safety step. And if your doctor suggests switching to another medication because of kidney concerns, it’s not a failure—it’s smart management. You’re not losing control of your diabetes; you’re adapting to protect your body.
The posts below cover real-world issues tied to this topic: how to read your lab results, what other drugs interact with metformin, how to talk to your doctor about dosage changes, and why generic versions work just as well. You’ll find advice on managing diabetes with kidney disease, spotting early signs of trouble, and avoiding dangerous combinations like metformin with contrast dyes or certain antibiotics. This isn’t theoretical—it’s what people actually deal with every day.
Updated 2025 guidelines for metformin and SGLT2 inhibitor dosing in kidney disease. Learn when to adjust doses, when to stop, and how to navigate conflicting FDA labels and clinical evidence.
View More