Metformin Renal Dosing: What You Need to Know About Kidney Safety and Dosage
When you take metformin, a first-line oral medication for type 2 diabetes that helps lower blood sugar by reducing liver glucose production and improving insulin sensitivity. It's one of the most prescribed drugs in the world—but its safety depends heavily on how well your kidneys are working. If your kidneys aren't filtering properly, metformin can build up in your body and raise the risk of a rare but serious condition called lactic acidosis. That’s why renal dosing, the adjustment of medication dosage based on kidney function isn’t just a technical detail—it’s a life-saving step.
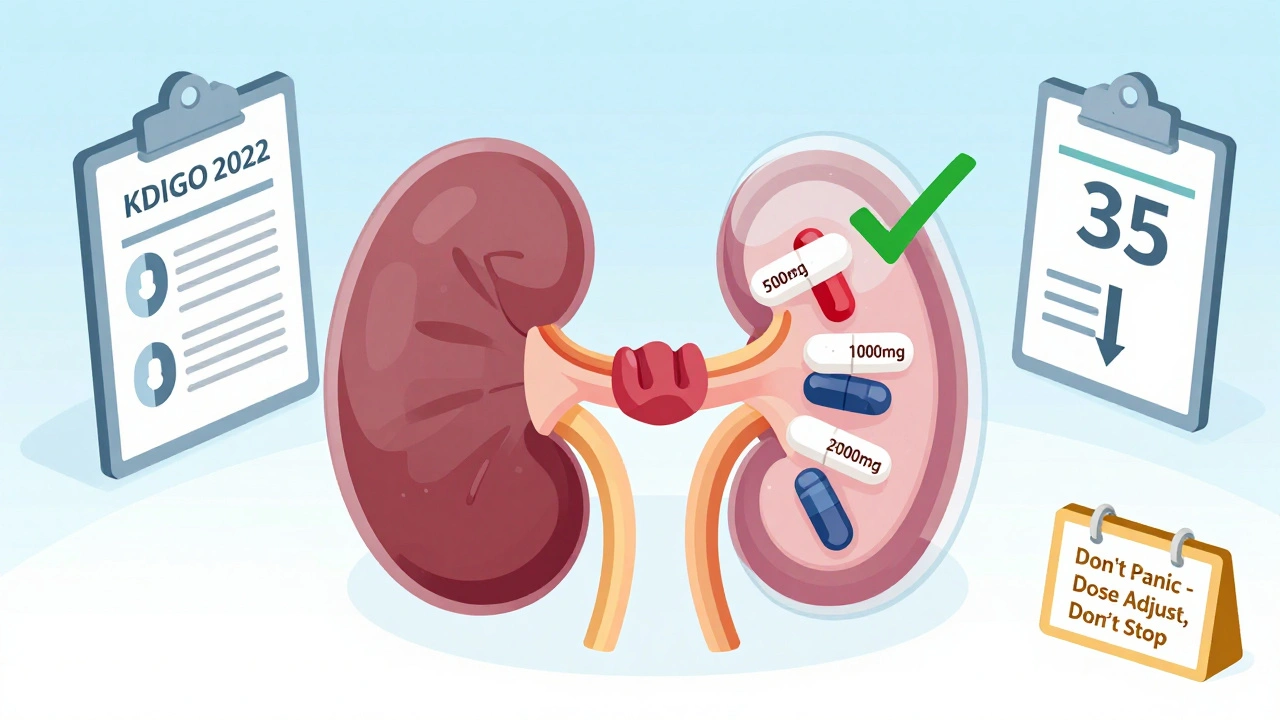
Your doctor doesn’t guess your kidney health. They check your eGFR, estimated glomerular filtration rate, a blood test that measures how well your kidneys filter waste. If your eGFR is below 45, most guidelines say to reduce your metformin dose. If it drops below 30, they’ll likely stop it altogether. This isn’t about being overly cautious—it’s about matching the drug to your body’s ability to clear it. People with diabetes often have other conditions like high blood pressure or heart disease, which can also affect kidney function. So even if your eGFR is borderline, your doctor might still adjust your metformin to stay safe.
It’s not just about the number on the lab report. Sometimes, your kidneys can look okay on paper but struggle under stress—like during an infection, dehydration, or after contrast dye for a scan. That’s why doctors ask you to hold metformin before certain procedures and restart it only after your kidneys are confirmed to be stable. Many patients don’t realize they need to pause their medication before a CT scan or X-ray with dye. Skipping that step can be dangerous.
And here’s something most people miss: metformin doesn’t damage kidneys. It’s the other way around—poor kidney function makes metformin risky. That’s why you’ll often see older adults on lower doses, not because they’re frail, but because kidney function naturally declines with age. The same dose that’s safe for a 40-year-old might be too much for a 70-year-old, even if they feel fine.
There are alternatives if metformin isn’t right for you. Drugs like SGLT2 inhibitors or GLP-1 agonists are now often preferred for people with kidney issues because they offer heart and kidney protection beyond just lowering blood sugar. But if metformin still works for you, and your kidneys are monitored, it remains one of the safest, cheapest, and most effective options out there.
What you’ll find in the posts below are real, practical guides on how to read your lab results, when to talk to your doctor about dosage changes, how other medications interact with metformin, and what to do if you’re worried about side effects. You’ll also see how kidney health connects to other common conditions—like dehydration, heart failure, and even common OTC painkillers. This isn’t theoretical. These are the things patients need to know to stay safe and in control of their care.
Updated 2025 guidelines for metformin and SGLT2 inhibitor dosing in kidney disease. Learn when to adjust doses, when to stop, and how to navigate conflicting FDA labels and clinical evidence.
View More