eGFR Guidelines for Diabetes: What You Need to Know
When you have diabetes, your eGFR, estimated glomerular filtration rate, is a key measure of how well your kidneys are filtering waste from your blood. Also known as estimated glomerular filtration rate, it’s not just a lab number—it’s an early warning system for kidney damage, which affects nearly 1 in 3 adults with diabetes. Doctors use eGFR to spot trouble before you feel symptoms, because by the time you’re tired, swollen, or urinating less, the damage may already be advanced.
Diabetes is the leading cause of kidney failure in the U.S., and eGFR is the main tool doctors use to monitor it. The eGFR guidelines for diabetes, recommend checking this number at least once a year for all patients with type 1 or type 2 diabetes. If your eGFR drops below 60 mL/min/1.73m² for three months or more, that’s a sign of chronic kidney disease. If it falls below 15, you’re approaching kidney failure. But here’s the thing: catching it early means you can slow or even stop the decline. Medications like SGLT2 inhibitors and GLP-1 agonists, which many people with diabetes already take for blood sugar, also protect the kidneys. That’s why tracking eGFR isn’t optional—it’s part of your diabetes management plan.
Your urine albumin-to-creatinine ratio, often called UACR, works with eGFR to give a full picture of kidney health. High albumin in your urine means your kidneys are leaking protein, another early sign of damage. Together, eGFR and UACR tell your doctor whether your kidneys are failing slowly or quickly, and whether your treatment needs to change. Many people don’t realize that high blood pressure, high cholesterol, and even some common painkillers like ibuprofen can make kidney damage worse. That’s why managing all three—blood sugar, blood pressure, and cholesterol—is just as important as checking your eGFR.
There’s no magic fix, but the data is clear: people who stick to their eGFR monitoring schedule, take their meds as prescribed, and make small lifestyle changes—like cutting back on salt, staying active, and avoiding smoking—have much better outcomes. You don’t need to be a doctor to understand your eGFR results. If your number drops, ask why. If your doctor doesn’t mention it, ask for it. Kidney damage from diabetes doesn’t happen overnight, but it doesn’t reverse itself either. The window to act is wide open—right now, while your kidneys still have room to recover.
Below, you’ll find real-world advice from people who’ve walked this path, along with guides on reading lab results, understanding medication impacts on kidneys, and avoiding common mistakes that speed up damage. These aren’t theory pieces—they’re practical tools built from patient experiences and clinical evidence.
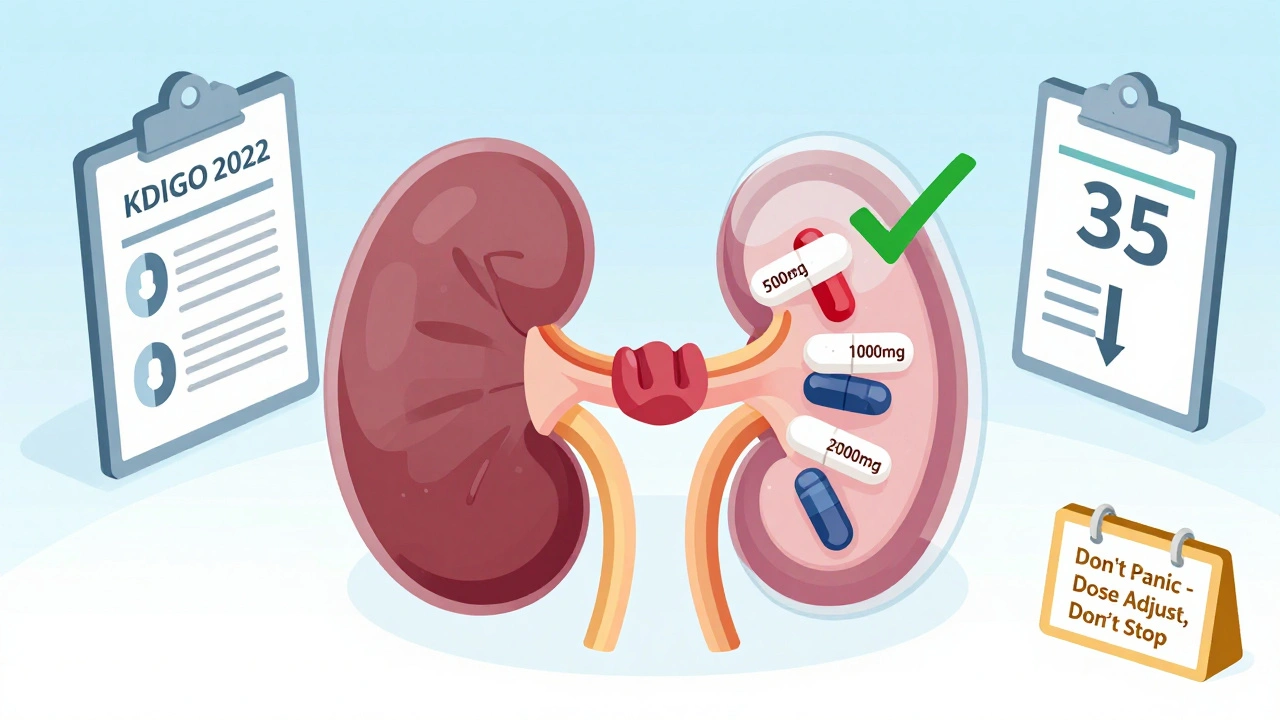
Updated 2025 guidelines for metformin and SGLT2 inhibitor dosing in kidney disease. Learn when to adjust doses, when to stop, and how to navigate conflicting FDA labels and clinical evidence.
View More