Rosacea Treatment Cost & Effectiveness Calculator
Your Treatment Options
Results
Select your treatment and location to see cost estimates and effectiveness comparison.
If you’re dealing with rosacea, you know how frustrating it can be. Redness, bumps, burning - it doesn’t just affect your skin, it affects your confidence. Soolantra, the brand name for topical ivermectin, has become a go-to for many people. But is it the best option? And are there cheaper, equally effective alternatives out there? Let’s cut through the noise and compare what actually works.
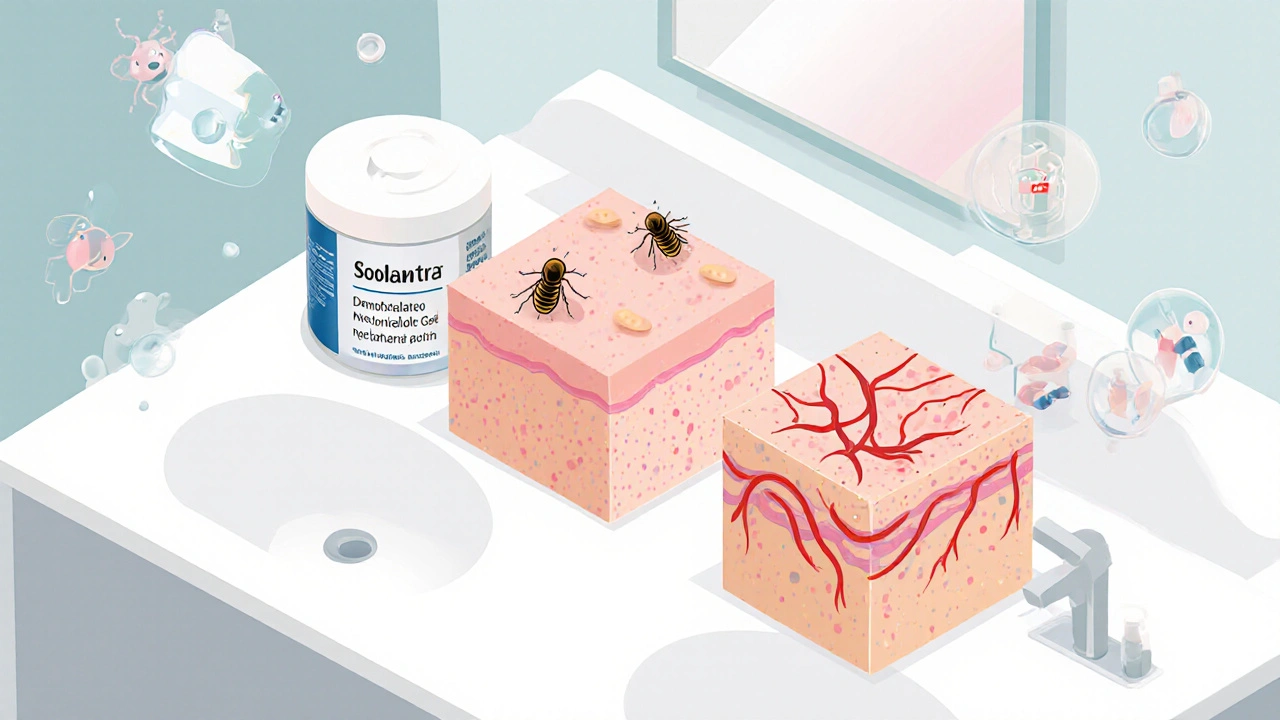
What is Soolantra, and how does it work?
Soolantra is a 1% topical cream containing ivermectin, approved by the TGA and FDA for treating inflammatory lesions of rosacea in adults. It was first introduced in 2014 and quickly became one of the most prescribed treatments for papulopustular rosacea. Unlike antibiotics or steroids, ivermectin doesn’t just kill bacteria - it targets the Demodex mites that live in your skin follicles. Research shows people with rosacea often have higher numbers of these mites, and their immune response to them triggers inflammation.
Most users start seeing results in 4 to 8 weeks. In clinical trials, about 40% of patients saw a 75% or greater reduction in lesions after 12 weeks. It’s not a quick fix, but for many, it’s a game-changer - especially when other treatments like metronidazole failed.
Top alternatives to Soolantra
There are several other topical and oral options for rosacea. Not all work the same way, and not all are suitable for everyone. Here are the most common alternatives.
Metronidazole (MetroGel, Rosadan)
Metronidazole is a topical antibiotic that’s been around for decades. It’s available as a gel, cream, or lotion, and is often the first-line treatment for mild to moderate rosacea. It reduces inflammation and kills bacteria, but it doesn’t directly target Demodex mites. Studies show it reduces lesions by about 30-50% over 9-12 weeks - less effective than ivermectin in head-to-head trials.
Pros: Cheaper, widely available, gentle on skin. Cons: Slower results, higher relapse rate after stopping. Many people switch to Soolantra after metronidazole stops working.
Azelaic Acid (Finacea, Skinoren)
Azelaic acid is a naturally occurring dicarboxylic acid derived from grains. It’s available as a 15% gel or 20% cream. It works by reducing inflammation, killing bacteria, and slowing down excess skin cell production. It’s also safe during pregnancy, which makes it a top pick for women.
In trials, azelaic acid reduced lesions by about 45% after 15 weeks. It’s slightly less effective than ivermectin but better tolerated by sensitive skin. Side effects? Mild stinging or redness at first - but it usually fades.
Brimonidine (Mirvaso)
Brimonidine is a topical alpha-2 agonist that temporarily shrinks blood vessels. It’s not for treating bumps or pimples - only for flushing and redness. It works in as little as 30 minutes and lasts up to 12 hours.
It’s great for quick fixes before events or photos. But it doesn’t treat the root cause. Rebound redness is common after stopping, and some users report worsening symptoms over time. It’s often used alongside Soolantra or azelaic acid for a two-pronged approach.
Oral Antibiotics (Doxycycline, Minocycline)
Low-dose doxycycline (40 mg delayed-release, sold as Oracea) is FDA-approved for rosacea. It’s an anti-inflammatory, not an antibiotic at this dose. It’s used for moderate to severe cases, especially when there’s widespread inflammation or eye involvement.
Results show 50-70% improvement in lesions after 12 weeks. But long-term use raises concerns about antibiotic resistance and gut health. Most dermatologists recommend it for short-term control, then switching to topical treatments like Soolantra for maintenance.
Isotretinoin (Accutane)
Isotretinoin is a powerful oral retinoid, usually reserved for severe acne. But it’s sometimes used off-label for severe, treatment-resistant rosacea. It reduces oil production and inflammation dramatically. Some patients see near-complete clearance.
But the side effects are serious: dry skin, lips, eyes; mood changes; liver stress; and it’s strictly off-limits during pregnancy. It’s not a first choice - only for extreme cases under close medical supervision.
Comparison: Soolantra vs Alternatives
| Treatment | Active Ingredient | Targets | Time to See Results | Effectiveness (Lesion Reduction) | Side Effects | Cost (AUD/month)* |
|---|---|---|---|---|---|---|
| Soolantra | Ivermectin 1% | Demodex mites, inflammation | 4-8 weeks | 70-75% | Mild burning, dryness | $80-$120 |
| Metronidazole | Metronidazole | Bacteria, mild inflammation | 6-12 weeks | 30-50% | Stinging, redness | $20-$40 |
| Azelaic Acid | Azelaic acid 15-20% | Inflammation, skin cells, bacteria | 8-12 weeks | 40-50% | Stinging, peeling (early) | $60-$90 |
| Brimonidine | Brimonidine tartrate | Redness only | 30 minutes | Redness: 50-60% | Rebound redness, flushing | $100-$140 |
| Low-dose Doxycycline | Doxycycline 40mg | Inflammation | 4-8 weeks | 50-70% | GI upset, sun sensitivity | $40-$70 |
| Isotretinoin | Isotretinoin | Oil glands, inflammation | 3-6 months | 70-90% | Severe: dryness, mood, liver | $50-$100 |
*Approximate out-of-pocket cost in Australia after PBS subsidy where applicable. Prices vary by pharmacy and brand.
Who should use Soolantra?
Soolantra shines for people with persistent inflammatory rosacea - the kind with red bumps and pustules that don’t respond to antibiotics or gentle creams. If you’ve tried metronidazole and it stopped working, Soolantra is often the next logical step.
It’s also a good choice if you want to avoid long-term antibiotics. Because it targets mites, not bacteria, there’s less risk of resistance. Many patients use it long-term with no loss of effectiveness.
It’s not ideal for pure redness without bumps. If your main issue is flushing, brimonidine or laser treatments might be better. And if you’re pregnant or breastfeeding, azelaic acid is safer.

Who should avoid Soolantra?
Soolantra is generally safe, but not for everyone. Avoid it if you:
- Have a known allergy to ivermectin or any ingredient in the cream
- Are using other strong topical treatments like retinoids or benzoyl peroxide at the same time - they can irritate skin further
- Have very sensitive or broken skin - apply only to intact skin
Some people report a temporary flare-up in the first 2 weeks. That’s normal - your skin is reacting to the mite die-off. Don’t stop unless it becomes unbearable.
Real-world experience: What patients say
One woman in Brisbane, 42, tried metronidazole for 8 months with little improvement. She switched to Soolantra and saw her bumps reduce by 80% in 10 weeks. She still uses it twice a week for maintenance.
A man in Melbourne, 58, had rosacea for 15 years. He tried everything - lasers, antibiotics, herbal creams. Soolantra was the first thing that gave him lasting relief. He says, "It didn’t cure me, but it gave me back my confidence."
On the flip side, some users find it too expensive. Others say it doesn’t touch their redness. That’s why combination therapy is often the key.
Combination therapy: The smart approach
Most dermatologists don’t rely on just one treatment. A common plan:
- Start with Soolantra to target mites and bumps
- Add brimonidine in the morning for redness
- Use gentle, fragrance-free moisturizers daily
- Avoid triggers: spicy food, alcohol, extreme heat, harsh cleansers
Some patients add azelaic acid at night if they still have lingering inflammation. Others use low-dose doxycycline for 3 months, then taper off to topical-only.
The goal isn’t perfection - it’s control. Rosacea can’t be cured, but it can be managed.
What about natural remedies?
Tea tree oil, aloe vera, green tea extracts - they’re popular online. But here’s the truth: there’s no strong evidence they work better than placebo for moderate to severe rosacea.
Some people swear by diluted tea tree oil (5%) for mites, but it can irritate skin. A 2023 study in the Journal of Clinical and Aesthetic Dermatology found tea tree oil was less effective than ivermectin and caused more irritation.
Don’t replace proven treatments with unproven ones. Natural doesn’t mean safe or effective. Use them only as gentle supports - not as primary therapy.
How to get Soolantra in Australia
Soolantra is available on the Pharmaceutical Benefits Scheme (PBS), so if you have a Medicare card, you pay around $30 per tube (or $7.70 for concession holders). Without PBS, it can cost over $150.
You need a prescription from a GP or dermatologist. Bring photos of your skin and a list of what you’ve tried. If your doctor says no, ask for a referral - dermatologists have more experience with rosacea treatment protocols.
Final thoughts: Is Soolantra worth it?
Soolantra isn’t the cheapest option. But it’s one of the most effective for inflammatory rosacea. If you’ve tried other treatments and they didn’t stick, it’s worth a shot.
It’s not magic. It takes time. It requires consistency. But for many, it’s the difference between hiding your face and living without fear.
Work with your doctor. Don’t give up after one failed treatment. And remember - rosacea isn’t your fault. You’re not broken. You just need the right tools.
Is Soolantra better than metronidazole for rosacea?
Yes, for inflammatory rosacea with bumps and pustules. Clinical trials show Soolantra (ivermectin) reduces lesions by 70-75% after 12 weeks, compared to 30-50% for metronidazole. Soolantra also targets Demodex mites, which metronidazole doesn’t. If metronidazole stopped working for you, Soolantra is the next step.
Can I use Soolantra every day?
Yes. Soolantra is designed for daily use - once a day, applied to the entire affected area. Most people use it long-term. Studies show no loss of effectiveness over 52 weeks. Some switch to every other day or 3 times a week after achieving control, but daily use is standard.
Does Soolantra help with redness?
Not directly. Soolantra targets inflammation caused by mites, which can reduce redness over time. But if your main symptom is persistent flushing or visible blood vessels, you’ll need something like brimonidine or laser therapy. Many people use Soolantra and brimonidine together for full coverage.
How long does it take for Soolantra to work?
Most people see improvement in 4 to 8 weeks. Full results usually take 12 weeks. Don’t stop early if you don’t see instant results. The mites die slowly, and inflammation fades gradually. Some see a temporary flare-up in the first 2 weeks - that’s normal and means it’s working.
Is there a generic version of Soolantra?
No, not yet. Ivermectin 1% cream is still under patent protection in Australia. Generic versions may become available after 2027. Until then, you can save money by using the PBS subsidy - pay only $30 per tube with a prescription.
Can I use Soolantra with other skincare products?
Yes, but be careful. Avoid strong actives like retinoids, glycolic acid, or benzoyl peroxide on the same area - they can cause irritation. Use Soolantra at night, and in the morning stick to gentle cleansers and moisturizers. Always patch test new products.
Next steps if you’re considering Soolantra
- Take clear photos of your skin - before and after any treatment
- Keep a trigger journal: what you eat, where you go, what you use on your face
- Ask your doctor for a referral to a dermatologist if you’ve tried two treatments without success
- Check if you qualify for the PBS subsidy - you may pay less than you think
- Don’t rush. Rosacea management is a marathon, not a sprint.
You’ve already taken the hardest step - you’re looking for answers. Now it’s about finding the right combination for your skin. Soolantra might be it. But even if it’s not, you’re not starting from zero. You’re one step closer to control.


Zac Gray
November 19, 2025 AT 01:39Soolantra isn't magic, but it's the closest thing we've got for stubborn rosacea bumps. I tried metronidazole for a year-zero results. Switched to Soolantra, and after 10 weeks, my face stopped looking like a chili pepper. Still use it twice a week now for maintenance. No rebound. No resistance. Just quiet skin.
Don't let the price scare you. If you're in Australia, PBS cuts it to $30. That's cheaper than your monthly coffee habit. Worth every cent if it gets you out of the house without a scarf.
Paige Lund
November 20, 2025 AT 02:16Wow. So Soolantra’s the new holy grail now? Next you’ll tell me tea tree oil is a myth and sunlight is a villain.
Just saying-I used nothing but aloe vera for two years and my skin improved. Coincidence? Maybe. But I’ll take my natural ‘cure’ over a prescription that costs more than my phone bill.
Ellen Calnan
November 21, 2025 AT 04:05I used to think rosacea was just ‘fair skin being dramatic.’ Then I got it. Now I understand why people cry in the mirror.
Soolantra didn’t fix me-but it gave me back the ability to look in the mirror without wanting to scream. That’s not treatment. That’s liberation.
And yes, the first two weeks felt like my face was being scraped with sandpaper. But that’s the mites dying. Don’t quit then. That’s when you’re winning.
Stop chasing perfection. Chase control. And if you’re using benzoyl peroxide on top of this? You’re not brave-you’re stupid. I’ve seen it. Your skin will revolt.
Also-PBS is your friend. If your GP says no, go to a dermatologist. Don’t let bureaucracy steal your confidence.
Brian Rono
November 22, 2025 AT 11:45Let’s be real: Soolantra works because it kills mites, not because it’s some miracle drug. The real scandal? We’ve known about Demodex mites in rosacea since the 1940s. But Big Pharma waited until they could patent a 70-year-old compound to make a billion. Ivermectin was used for river blindness in Africa. Now it’s a luxury cream for rich white people with sensitive skin.
And don’t get me started on brimonidine. That’s just a chemical trick to hide redness. Like putting tape over a leaking pipe. Rebound redness? Of course. Your blood vessels are screaming for mercy.
Meanwhile, azelaic acid is cheaper, pregnancy-safe, and doesn’t require a PhD to pronounce. Why isn’t this the first-line treatment? Because it can’t be patented. Simple as that.
Richard Risemberg
November 23, 2025 AT 23:22For anyone reading this and thinking, ‘I’ve tried everything’-you’re not broken. You’re just on the wrong path.
I was in the same boat. Tried lasers, antibiotics, herbal tonics, even a $200 ‘anti-rosacea’ serum that smelled like wet socks. Nothing worked.
Soolantra didn’t fix me overnight. But after 12 weeks, the bumps? Gone. The burning? Gone. The shame? Still there, but fading.
Here’s the secret: it’s not about one product. It’s about the combo. Soolantra at night, gentle moisturizer in the morning, brimonidine before a date, and NO alcohol, NO spicy food, NO hot showers. It’s a lifestyle. Not a pill.
And yes-PBS makes it affordable. If your doctor won’t prescribe it, go to another. Your skin deserves better than a sales pitch.
Michael Salmon
November 25, 2025 AT 12:50Everyone’s acting like Soolantra is the second coming. Newsflash: 40% of people in the trials didn’t hit 75% improvement. That’s more than half. And the rest? They’re just posting selfies with #SoolantraSuccess while their skin is still on fire.
And don’t even get me started on the ‘it’s not an antibiotic’ marketing. Ivermectin is an antiparasitic. You’re literally poisoning your skin with a dewormer. That’s not science-that’s desperation.
Meanwhile, azelaic acid has been used since the 1980s. It’s natural, safe, and doesn’t require a PhD to pronounce. But nope-we need a $120 tube of ‘revolutionary’ mite murder.
Christopher Robinson
November 26, 2025 AT 14:54As someone who’s had rosacea since 18, I’ve tried it all. Even the ‘miracle’ oatmeal masks from Etsy.
Soolantra was the first thing that actually *stuck*. But here’s the thing-it’s not the product. It’s the routine. I use it every night, no exceptions. I don’t touch my face. I wash with lukewarm water. I use a humidifier. I stopped drinking wine.
It’s not glamorous. But it works.
And if you’re worried about cost? PBS is real. Ask for the concession rate. You’re not being lazy-you’re being smart.
Also-brimonidine is great for events. I use it before work meetings. But I never rely on it alone. It’s a tool, not a cure.
You’re not alone. We’re all just trying to look like ourselves again.
Reema Al-Zaheri
November 27, 2025 AT 00:27Regarding the comparison table: the cost figures for Soolantra are misleading. In the U.S., without PBS, it's approximately $150 per tube, but with insurance, it's often covered under Tier 3 or 4. In Australia, the PBS subsidy reduces it to $30.40 for general patients and $7.70 for concession cardholders. This is critical context. The efficacy data is accurate, but cost perception is skewed without this clarification.
Additionally, the long-term safety profile of ivermectin 1% cream is well-documented in studies extending beyond 52 weeks, with no significant systemic absorption. Topical application is localized. Please do not conflate it with oral ivermectin used for parasitic infections.
seamus moginie
November 27, 2025 AT 16:04I’m from Ireland. I’ve lived with this for 17 years. I’ve been to six dermatologists. I’ve spent thousands. I’ve cried in pharmacies because I couldn’t afford the cream.
Then I got Soolantra through a clinical trial. I didn’t believe it. I thought it was a scam. But after six weeks? My skin looked like it did when I was 14. No redness. No bumps. No hiding.
Now I pay $30 a month. I’d pay $300. This isn’t skincare. This is my dignity.
If you’re hesitating because of cost-apply for PBS. If your doctor won’t help-go to another. If you’re scared of side effects-start slow. One dot on your chin. Wait three days. Then move on.
You’re not weak for needing help. You’re brave for looking for it.
James Ó Nuanáin
November 29, 2025 AT 09:28While I appreciate the clinical overview, the omission of British NICE guidelines is a glaring oversight. The National Institute for Health and Care Excellence does not recommend ivermectin as first-line therapy in the UK due to insufficient cost-effectiveness data relative to azelaic acid and metronidazole.
Furthermore, the suggestion that Soolantra is ‘the next logical step’ after metronidazole is not universally supported by UK dermatological consensus. In fact, the British Association of Dermatologists advises a stepped-care approach, with laser therapy for persistent erythema preceding prescription topical agents.
Additionally, the claim that ivermectin has ‘no resistance risk’ is scientifically dubious. Resistance mechanisms in Demodex folliculorum are currently under investigation, and overuse may accelerate adaptation.
One must question the commercial influence behind the promotion of this product in public discourse.
Nick Lesieur
November 30, 2025 AT 17:38So you’re telling me I should pay $120 for a cream that makes my face tingle like I licked a battery... but it kills mites?
Meanwhile, my cousin in Ohio uses coconut oil and says his skin’s ‘better than ever.’
Also, why is everyone acting like this is the first time anyone’s ever had red skin? My grandma had rosacea in the 50s. She used witch hazel. Lived to 92.
Maybe the real problem is we’ve forgotten how to just... chill.
Steve and Charlie Maidment
December 1, 2025 AT 00:12Why does everyone act like Soolantra is the answer? I’ve been using it for 6 months. My bumps are gone. But my redness? Worse than ever. And now my skin feels like sandpaper.
And don’t get me started on the cost. I’m on disability. $30 is still too much when I’m choosing between food and face cream.
Also, why is no one talking about how the ‘mite theory’ is still just a theory? I’ve read the papers. It’s correlation, not causation.
Meanwhile, I’ve got a $5 jar of sulfur cream that’s been sitting in my cabinet for 3 years. Maybe I should’ve just stuck with that.
Codie Wagers
December 1, 2025 AT 10:12Let’s be honest: this entire thread is just a well-crafted advertisement disguised as medical advice. Ivermectin? A dewormer. Azelaic acid? A grain derivative. Brimonidine? A vasoconstrictor with rebound effects.
What’s missing? The real root cause: systemic inflammation from gut dysbiosis, stress, and environmental toxins. But no-let’s just slap a $120 cream on our faces and call it a day.
You’re treating symptoms. Not the disease.
And the fact that you’re all praising a pharmaceutical product while dismissing natural remedies? That’s not science. That’s corporate worship.
Next time, ask: who profits? Not ‘what works.’
Angela Gutschwager
December 2, 2025 AT 23:55I used Soolantra. It worked. Then I stopped. Now my skin is back to looking like a tomato. I’m not mad. Just tired.
Also, why is everyone so dramatic about the price? It’s $30. I spend that on takeout twice a week.
And yes, I use it with brimonidine. And yes, I avoid spicy food. And no, I don’t care if you think it’s overhyped.
I just want to look in the mirror without wanting to cry.
Michael Petesch
December 3, 2025 AT 13:05As someone who grew up in India and now lives in the U.S., I’ve seen rosacea treated very differently across cultures. In Delhi, dermatologists often start with azelaic acid or oral tetracycline. In Texas, it’s Soolantra on day one.
It’s not about which treatment is better-it’s about access, culture, and pharmaceutical influence. In the U.S., direct-to-consumer ads shape expectations. In India, cost and availability dictate treatment.
But the science? It’s universal. Demodex mites are real. Inflammation is real. And yes, Soolantra works for many.
But let’s not pretend this is a one-size-fits-all solution. Skin is personal. Culture is personal. Treatment should be too.
Brian Rono
December 4, 2025 AT 15:25Oh, so now we’re calling Soolantra ‘the solution’? Let me guess-the next comment will be ‘I used it and my skin glowed!’
Meanwhile, the real issue? The fact that dermatologists are trained to prescribe, not to educate. No one told me to track triggers. No one said ‘avoid heat.’ No one warned me about rebound redness from brimonidine.
They just handed me a tube and said ‘use this.’
And now we’re acting like it’s a miracle because it worked for one person?
Wake up. This isn’t medicine. It’s marketing with a prescription pad.