Peritoneal Dialysis at Home: CAPD vs. APD - What You Need to Know
If you’re living with kidney failure, dialysis isn’t just a medical procedure-it’s a lifestyle. And for many people, doing it at home is the only way to keep some control over their daily lives. Two main types of peritoneal dialysis (PD) are available: Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD). Both use your abdominal lining to clean your blood, but how they work, what they require, and how they fit into your life couldn’t be more different.
Neither is better for everyone. The right choice depends on your health, your routine, your home setup, and even how you sleep. Let’s break down the real differences-not just the clinical terms, but what it actually feels like to live with each one.
How CAPD Works: Manual Exchanges, No Machine Needed
CAPD has been around since the 1970s. It’s simple in design: you manually fill your abdomen with dialysis fluid, let it sit for a few hours, then drain it out. You do this 3 to 5 times a day, every day. Each exchange takes about 30 to 40 minutes. No machines. No electricity. Just gravity, clean hands, and a quiet spot to work.
You carry your dialysis bags with you. Most people keep them in a small bag or backpack. A typical day might look like this: you do one exchange when you wake up, another during your lunch break, one after dinner, and one before bed. Some people even do one while sitting on the couch watching TV. The fluid stays in your belly for 4 to 6 hours each time, slowly pulling out waste and extra fluid.
It sounds straightforward, but it’s physically demanding. You need good hand strength and fine motor skills to handle the tubing and connect/disconnect the bags without contamination. If you have arthritis, shaky hands, or trouble bending over, CAPD can become a daily struggle. And because you’re doing it yourself, every exchange carries a risk of infection-especially peritonitis, which happens when bacteria get into your abdomen. Studies show CAPD users average 0.68 episodes of peritonitis per year, slightly higher than APD users.
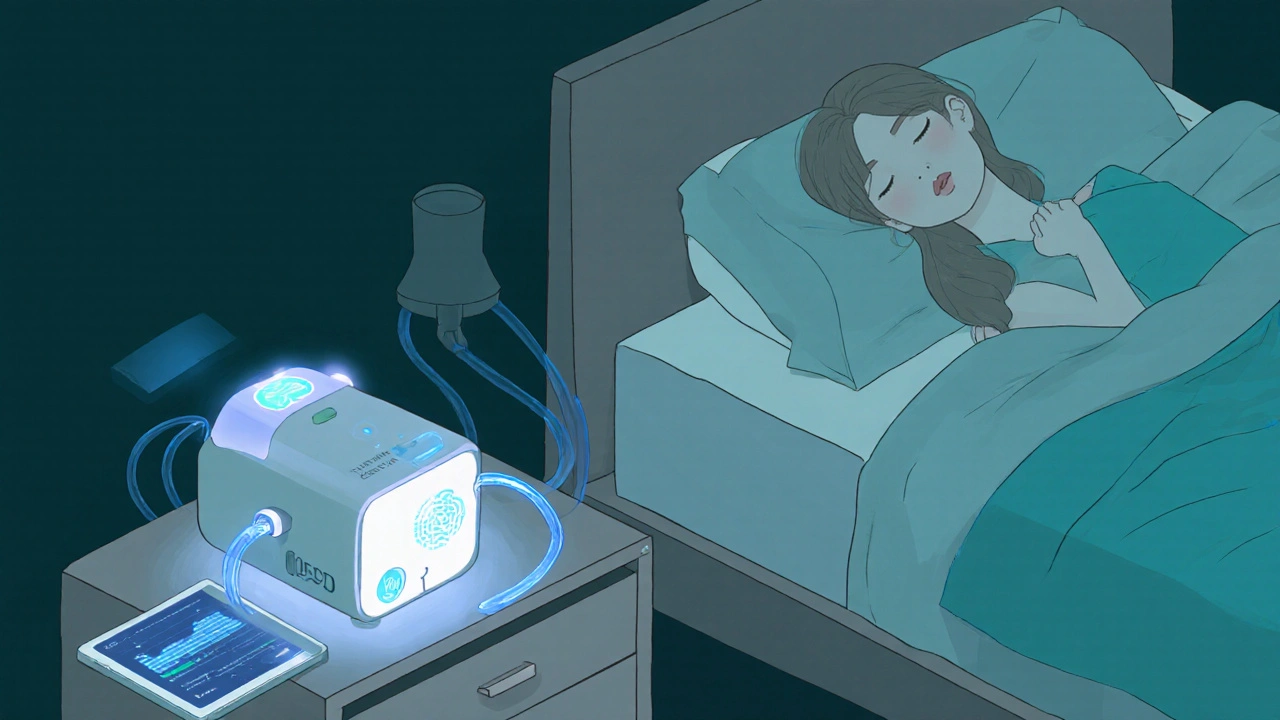
How APD Works: Sleep While the Machine Does the Work
APD flips the script. Instead of doing exchanges during the day, you hook up to a machine-called a cycler-before bed. The machine automatically fills your belly with fluid, lets it sit, then drains it out over 8 to 10 hours while you sleep. You wake up with your abdomen empty and ready to go about your day without any dialysis interruptions.
The machines are compact-about the size of a small suitcase, weighing 15 to 25 pounds. You need a dedicated electrical outlet and a little floor space near your bed. Modern cyclers like the Baxter Amia or Fresenius Sleep-Safe come with safety features: they detect air bubbles, monitor pressure, and even shut down if something goes wrong. Some even connect to your phone or tablet so your care team can check your treatment data remotely.
Because the exchanges happen overnight, you’re free during the day. That’s why APD is popular with working adults, parents, and anyone who wants to avoid dialysis interruptions. Mayo Clinic data shows APD users get an average of 3.2 more hours of sleep per night than CAPD users. That’s not just comfort-it’s real quality-of-life improvement.
But it’s not without downsides. If the machine breaks down in the middle of the night, you’re stuck. About 12% of APD users experience a cycler malfunction each year. Some report the noise-around 35 to 45 decibels, like a quiet library-as disruptive, even with earplugs. And if you’re traveling, you’ve got to pack the machine, find an outlet, and set it up every time.
Costs and Insurance: What You’ll Actually Pay
Both CAPD and APD are covered by Medicare in the U.S., with 80% of costs paid by the government. But what you pay out of pocket depends on the modality.
CAPD supplies-bags, tubing, disinfectants-cost about $50 to $75 per month. APD supplies are similar, but you also pay for the cycler rental. That adds $25 to $50 more per month, bringing APD’s out-of-pocket cost to $75 to $100. That might seem like a big difference, but here’s the catch: APD users often need fewer medications. Better fluid control means less high blood pressure, fewer diuretics, and lower phosphorus levels. One study found APD reduced long-term medication costs by 15 to 20%.
Insurance policies vary. In some European countries, APD gets higher reimbursement to encourage its use. In Australia and Canada, home dialysis is strongly supported, and both CAPD and APD are fully covered with minimal patient cost. But in rural U.S. areas, access to training and equipment delivery can be a real barrier.
Who’s Better Off With CAPD?
CAPD isn’t outdated-it’s just different. It’s ideal for people who:
- Have limited space at home (no need for a machine)
- Travel often or live in places with unreliable electricity
- Prefer to be in control of every step of their treatment
- Are over 75 and have cognitive or physical limitations that make machine use risky
Dr. Michael J. Germain, a nephrologist and past president of the American Society of Nephrology, says CAPD remains the gold standard for patients over 75 because it’s easier to learn and doesn’t rely on technology that can fail. If you’re retired, live alone, and don’t want to deal with tech support calls at 2 a.m., CAPD gives you independence without complexity.
It’s also better if you still have some kidney function-more than 2 mL/min of urine output. CAPD’s continuous filtering helps preserve that remaining function longer than APD’s batch-style treatment.
Who’s Better Off With APD?
APD shines for people who want their treatment to fit into their life-not the other way around. It’s the top pick for:
- Working adults who can’t afford daytime dialysis breaks
- People who struggle with manual dexterity (arthritis, Parkinson’s, tremors)
- Those who want better sleep and fewer daytime disruptions
- Patients with fluid overload or high blood pressure-APD controls these better
A 2021 meta-analysis found APD users had 22% fewer episodes of dangerous fluid overload compared to CAPD users. That means fewer hospital trips, less strain on the heart, and better long-term outcomes.
Also, modern APD machines come with remote monitoring. Your nurse can see if your treatment ran correctly, if fluid levels are off, or if you missed a cycle-all without you calling in. That’s a game-changer for safety. In fact, programs with remote monitoring cut emergency visits by 25%.
Training and Support: The Real Hurdle
Training for either method isn’t quick. CAPD usually takes 10 to 14 days of daily instruction. You learn sterile technique, how to connect tubing, how to spot signs of infection, and how to handle emergencies like a disconnected line.
APD training takes longer-14 to 21 days-because you’re learning a machine. You’ll practice setting up the cycler, loading bags, troubleshooting error codes, and handling power outages. You’ll also learn how to switch to manual exchanges if the machine fails.
Support differs too. About 95% of APD programs offer 24/7 technical support. If your cycler beeps at midnight, you can call and get help fast. CAPD support is more clinical-you call for infection concerns or technique issues, but there’s no “machine repair” hotline.
Both need regular check-ins: monthly nurse visits, quarterly doctor visits. But APD’s remote monitoring means fewer in-person trips. That’s a big plus if you live far from a dialysis center.

Real People, Real Stories
On patient forums, the differences come alive.
DialysisDave, a 58-year-old teacher in Ohio, says: “I’ve done CAPD for seven years. I do my exchanges during my planning period. No machine. No noise. Just me and my bag. I’ve traveled to Europe with it-no problem.”
NightNurse82, a 42-year-old ER nurse in Texas, says: “APD lets me work 12-hour shifts without stopping. I sleep, the machine works. But I’ve had three cycler breakdowns in two years. One was at 3 a.m. I had to do manual exchanges until the tech came. It’s stressful.”
Reddit users report CAPD users love the freedom to move but hate the daytime interruptions. APD users love the sleep and freedom during the day but dread machine issues. It’s not about which is better-it’s about which fits your life.
What the Future Holds
Technology is moving fast. Baxter’s Amia system, launched in 2021, uses AI to adjust your dialysis prescription based on your weight and blood pressure. In trials, it cut fluid overload events by 31%. By 2025, the first smartphone-connected cycler will be FDA-approved-reducing setup errors by 40%.
Meanwhile, CAPD isn’t being left behind. New, lighter bags and easier-to-use connectors are making manual exchanges simpler. But the trend is clear: APD adoption is growing at 7.3% per year. CAPD grows at just 2.1%. By 2030, APD will likely make up 65% of home PD cases.
Still, CAPD will always have a place. For older adults, those without reliable power, or those who just don’t trust machines, it’s a reliable, low-tech lifeline.
Final Decision: Ask Yourself These Questions
Choosing between CAPD and APD isn’t just about medical stats. It’s about your daily reality. Ask yourself:
- Do I have space for a machine? Do I have a reliable power source?
- Can I handle small tubes and bags with my hands? Do I have arthritis or tremors?
- Do I work nights or irregular hours? Do I travel often?
- Am I okay with a machine breaking down? Can I handle a backup plan?
- Do I want to be in control of every exchange-or let the machine do it while I sleep?
- Do I have someone who can help me if things go wrong?
There’s no one-size-fits-all answer. The best dialysis is the one you can stick with. Talk to your care team. Try a trial week with each method if possible. Your life, your body, your rules.
Can I switch from CAPD to APD later if I change my mind?
Yes, you can switch between CAPD and APD at any time. Many people start with CAPD because it’s simpler, then move to APD once they get used to home dialysis and want more freedom. Others start with APD and switch to CAPD if their machine breaks down too often or if they lose access to electricity. Your care team will guide you through the transition, including retraining and adjusting your treatment plan.
Is one method safer than the other?
Both carry risks, but different ones. CAPD has a slightly higher risk of peritonitis because you’re handling the tubing multiple times a day. APD reduces that risk by automating exchanges, but introduces risks from machine failure, power outages, or improper setup. Modern APD machines have safety features that lower these risks significantly. Overall, both are safe when done correctly-with proper training and hygiene.
What happens if my APD machine breaks down?
Every APD program provides backup supplies and training for manual exchanges. If your cycler fails, you switch to CAPD-style exchanges until it’s fixed. Most machines have a manual mode or emergency setting. If it happens at night, you call your 24/7 support line-they’ll guide you through the backup process and send a replacement part or unit within 24 hours. It’s rare for someone to miss a full day of dialysis.
Can I travel with either type of peritoneal dialysis?
Yes, both are travel-friendly, but differently. CAPD is easier-you just pack your dialysis bags and supplies in a cooler. You can do exchanges in hotel rooms, airports, or even rest stops. APD requires you to bring the cycler, find an outlet, and set it up. Some newer cyclers are battery-powered or work with car adapters. Many dialysis suppliers offer shipping services to send supplies to your destination ahead of time.
Which method gives me better long-term survival?
Studies show no major difference in long-term survival between CAPD and APD. Both have similar 5-year survival rates-around 52% to 58%. What does make a difference is sticking with the treatment. People who miss exchanges or skip training have worse outcomes, no matter which method they use. APD may reduce hospitalizations for fluid overload, which helps preserve heart health, but the biggest factor is consistency.


Sam Jepsen
November 23, 2025 AT 19:29For anyone thinking about switching, just try both for a week. Your body will tell you what it needs.
Yvonne Franklin
November 25, 2025 AT 05:42Justin Daniel
November 25, 2025 AT 19:42Melvina Zelee
November 26, 2025 AT 16:48tech is great. but sometimes simple just works better.
ann smith
November 28, 2025 AT 04:12It’s not about which is better - it’s about which lets you live.
Keep going. You’re stronger than you think. 💪
Julie Pulvino
November 29, 2025 AT 10:12It’s not one size fits all. It’s one size fits YOU.
Patrick Marsh
December 1, 2025 AT 00:55Danny Nicholls
December 1, 2025 AT 13:50yeah the machine broke once. but i learned how to do it manually. and the nurse sent a new one in 10 hours.
also the app tells me when i’m off on fluid. it’s like a fitness tracker for my kidneys 😅
Mark Williams
December 3, 2025 AT 06:20Longitudinal data suggests APD’s nocturnal dwell volume optimization reduces interdialytic weight gain, lowering cardiovascular strain. However, the risk of mechanical failure introduces a non-biological variable that may compromise adherence.
Daniel Jean-Baptiste
December 4, 2025 AT 02:56apd sounds nice but what if the power goes out for 2 days in winter? capd dont care. its just bags and hands. simple. reliable.
tech is cool but sometimes old school is the real innovation.
Ravi Kumar Gupta
December 4, 2025 AT 03:59Stop talking about ‘preferences’. For many of us, it’s not a choice - it’s survival. CAPD is the real MVP.
Rahul Kanakarajan
December 5, 2025 AT 10:34New Yorkers
December 5, 2025 AT 10:38CAPD? You’re a warrior. APD? You’re a tech bro.
Either way, you’re still on the grind. So stop arguing. Just live.