Itching from opioids isn’t always an allergy - and mistaking it for one can leave you in pain
If you’ve ever felt itchy after taking morphine or oxycodone, you’re not alone. Around 68% of people on these drugs report it. But here’s the catch: itching doesn’t mean you’re allergic. Most of the time, it’s just your body reacting to the drug’s chemistry - not your immune system. Yet, too many patients get labeled "allergic to opioids" because of this, and end up stuck with weaker pain relief, higher costs, or even untreated pain.
True opioid allergies? Rare. Less than 0.3% of people who take them have a real immune reaction. But up to 80% of the so-called "opioid allergies" reported in clinics are actually pseudoallergic reactions - meaning histamine gets released without any immune system involvement. This isn’t just a technical detail. It changes everything about how you’re treated.
What’s really happening when you get itchy?
When you take morphine or codeine, your body’s mast cells - tiny immune cells in your skin - get triggered directly by the drug. They dump histamine, which causes itching, flushing, sweating, or mild dizziness. It feels like an allergy, but your immune system didn’t learn to recognize the drug as a threat. No antibodies. No memory. Just a chemical reaction.
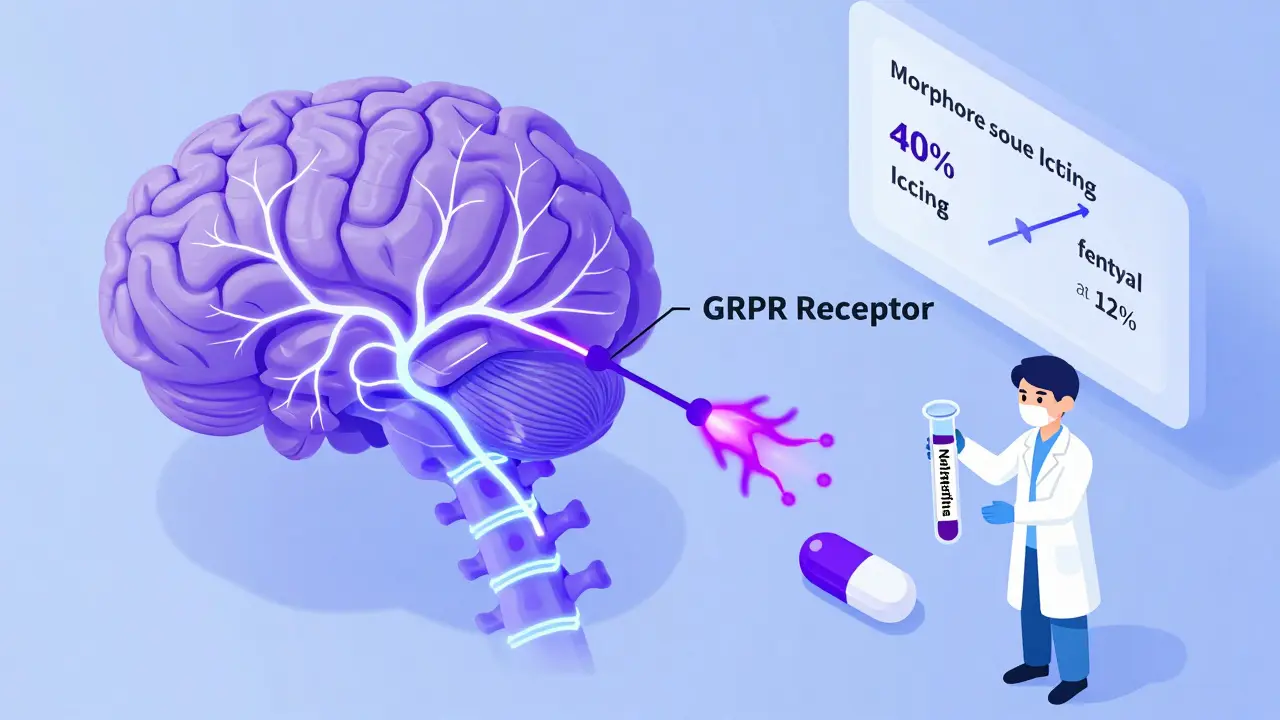
This is why the itching usually shows up within minutes, gets worse with higher doses, and improves if you slow down the infusion or lower the amount. Morphine releases about 3-4 times more histamine than an equal pain-relieving dose of hydromorphone. That’s why someone might itch badly on morphine but feel fine on fentanyl or methadone - they’re chemically different.
And here’s something surprising: some itching isn’t even from histamine. Research from Washington University found that opioids activate a specific receptor in your spinal cord - called GRPR - that directly causes itch signals to your brain. That’s why antihistamines like Benadryl sometimes don’t help at all. The itch is coming from inside your nerves, not your skin.
What does a real opioid allergy look like?
True allergic reactions are different. They’re rare, but dangerous. If you’ve ever had hives that spread quickly, swelling of your lips or tongue, trouble breathing, or a sudden drop in blood pressure after taking an opioid, that’s a red flag. These reactions usually happen fast - within minutes - and involve more than one system: skin and lungs and heart.
Doctors use this rule: if it’s just itching, nausea, or drowsiness, it’s likely not an allergy. If you’re wheezing, your throat is closing, or you feel like you’re going to pass out, that’s a medical emergency. These are IgE-mediated responses - your body has made antibodies against the drug, and now it’s attacking it. This kind of reaction can happen even on the first dose, but it’s extremely uncommon.
One case from Mayo Clinic involved a woman who went into anaphylaxis five minutes after her first morphine shot. Her blood pressure crashed to 70, her oxygen dropped, and she needed epinephrine and ICU care. That’s a real allergy. But it’s not the kind most people experience.

Why mislabeling opioids as allergies is a big problem
When you’re labeled "allergic to opioids," your doctors avoid giving you anything in that class - even if it’s the best option for your pain. That’s a problem. In cancer care, chronic pain, or after surgery, opioids are often the most effective tools we have.
A 2022 study at the University of Michigan found that 87% of patients who said they were "allergic to opioids" only had itching, nausea, or dizziness - not real allergy symptoms. Yet, they were denied effective pain relief. In palliative care, 78% of patients with this label were able to safely use other opioids after trying antihistamines or switching drugs.
The cost? About $1,200 extra per patient per year. Why? Because instead of morphine or oxycodone, they get expensive alternatives like tramadol or non-opioid combos that don’t work as well. In the U.S., this mislabeling adds up to $24-36 billion a year in unnecessary spending.
Electronic health records now have alerts to flag suspected pseudoallergies, and hospitals that use them have cut wrong allergy labels by 45%. But it still happens - because many providers aren’t trained to tell the difference.
What to do if you get itchy on opioids
If you’re itchy but not having trouble breathing or swelling, here’s what actually works:
- Don’t stop the opioid. You’re probably not allergic. Stopping it means you’re missing out on pain control.
- Ask for an antihistamine. Diphenhydramine (Benadryl) 25-50 mg IV or oral 30 minutes before your next dose cuts itching in 80-90% of cases.
- Lower the dose. Reducing the amount by 25-50% often makes the itching go away without losing pain relief.
- Try a different opioid. Switch from morphine or oxycodone to fentanyl or methadone. Fentanyl causes itching in only 10-15% of users vs. 30-40% with morphine. Methadone? Even less. Why? Their chemical structure doesn’t trigger mast cells the same way.
Some patients report that switching from oral morphine to a fentanyl patch makes all the difference. One Reddit user wrote: "I was told I’m allergic to all opioids because I got itchy on morphine. Fentanyl patch? Works fine with Benadryl. Why was I denied this for years?"
What if you really are allergic?
If you’ve had a true allergic reaction - swelling, breathing trouble, anaphylaxis - then yes, avoid that opioid and others like it. Morphine, oxycodone, and hydrocodone are all phenanthrenes and can cross-react. But fentanyl, meperidine, and methadone are chemically different and rarely cause cross-reactions (less than 5% risk).
For patients who need opioids but have a confirmed allergy, desensitization is an option. At specialized centers, doctors slowly give increasing doses over 4-6 hours under close watch. Success rates are above 95%. It’s not for everyone, but it’s life-changing for those who need strong pain control and have no other options.
New treatments on the horizon
Science is catching up. A new drug called nalfurafine - approved in Japan for years and in late-stage trials in the U.S. - targets the itch pathway directly without affecting pain relief. In trials, it reduced opioid-induced itching by 70%. Another drug, CR845 (korsuva), is also showing promise.
Researchers are even looking at genetics. Some people have variations in the HTR7 gene that make them more likely to release histamine when exposed to opioids. In the future, a simple blood test might tell you your risk before you even take the drug.
But for now, the most powerful tool is knowledge. If you’ve been told you’re allergic to opioids because you got itchy - ask your doctor: "Is this a true allergy, or a pseudoallergic reaction?" Show them this information. You might be able to get back to the pain relief you need.
Bottom line: Don’t assume itching means allergy
Itching from opioids is common. It’s not dangerous. It’s not an allergy. It’s a side effect - and one that’s easy to manage. Stopping your medication because of it might cost you more than just pain. It could cost you quality of life.
Use antihistamines. Lower the dose. Switch drugs. Talk to your provider. You don’t have to live with untreated pain because of a misunderstanding.
Is itching from opioids a sign of a true allergy?
No, itching alone is almost never a sign of a true opioid allergy. In fact, about 70-80% of people who report "opioid allergies" are actually experiencing pseudoallergic reactions - histamine release triggered directly by the drug, not an immune response. True allergies involve symptoms like swelling, trouble breathing, or low blood pressure, not just itching.
Can I still take opioids if I get itchy?
Yes, in most cases. You can often continue using opioids by lowering the dose, taking an antihistamine like diphenhydramine before dosing, or switching to a different opioid like fentanyl or methadone, which cause less histamine release. Only stop if you have signs of a true allergic reaction like swelling or breathing difficulty.
Which opioids cause the most itching?
Morphine and codeine cause the most itching because they strongly trigger histamine release. Oxycodone and hydrocodone are similar. Fentanyl, methadone, and hydromorphone cause far less itching - fentanyl releases about 3-4 times less histamine than morphine per equivalent pain-relieving dose.
Why do some people get itchy even after taking antihistamines?
Because not all opioid-induced itching comes from histamine. Research shows some itching is caused by opioids activating GRPR receptors in the spinal cord, which send itch signals directly to the brain. Antihistamines won’t help with this type - but drugs like nalfurafine, which target these receptors, are showing promise in clinical trials.
Should I get tested for an opioid allergy?
Routine skin testing isn’t recommended unless you had a severe reaction like anaphylaxis. Skin tests for opioids have high false-positive rates - up to 30% - and often don’t predict real risk. The best test is a supervised trial with a different opioid and antihistamine support. Most people labeled allergic can safely try alternatives.
What’s the safest opioid if I’ve had itching before?
Fentanyl and methadone are the safest choices. Fentanyl causes itching in only 10-15% of users compared to 30-40% with morphine. Methadone causes even less histamine release. Both are chemically different from morphine and rarely cross-react. However, methadone requires careful dosing due to its long half-life, and fentanyl is very potent - both need close monitoring.


Phil Hillson
January 19, 2026 AT 17:43Josh Kenna
January 20, 2026 AT 08:03Erwin Kodiat
January 21, 2026 AT 08:44Jacob Hill
January 22, 2026 AT 20:39Lewis Yeaple
January 24, 2026 AT 17:14Tracy Howard
January 24, 2026 AT 20:11Aman Kumar
January 25, 2026 AT 09:26Jake Rudin
January 25, 2026 AT 23:38