Bowel Function Index Calculator
Bowel Function Index Calculator
Track your opioid-induced constipation severity with this doctor-approved tool. A score above 30 indicates significant constipation that requires treatment adjustment.
Please rate your symptoms (0-10 scale):
Your Results
Bowel Function Index Score: 0
When you start taking opioids for chronic pain, you’re probably focused on relief - not constipation. But here’s the hard truth: opioid-induced constipation affects 40 to 60% of people on long-term opioids, and it doesn’t go away on its own. Unlike nausea or drowsiness, which often fade after a few weeks, constipation sticks around for as long as you’re on the medication. And if left unchecked, it can turn into something far worse - bloating, vomiting, fecal impaction, or even intestinal blockage.
Why Opioids Cause Constipation
Opioids don’t just block pain signals in your brain. They also latch onto receptors in your gut, specifically the μ-opioid receptors in the intestinal wall. This slows down the natural muscle contractions that push food and waste through your digestive tract. Your colon absorbs more water from stool, making it hard and dry. Your anal sphincter tightens up, making it harder to push out what’s there. The result? Straining, a feeling of incomplete emptying, and sometimes days without a bowel movement.This isn’t normal constipation. It’s mechanistically different. Over-the-counter remedies that work for occasional sluggish bowels often fail here because they don’t address the root cause: opioid receptors in your gut. That’s why simply doubling up on fiber or senna might not help - and why so many patients end up frustrated.
Prevention Is Key - Start Laxatives on Day One
The biggest mistake doctors and patients make? Waiting for constipation to happen before treating it. By the time you’re straining or feeling bloated, the process is already well underway. Experts agree: if you’re starting opioids, you should start a laxative at the same time.Studies show that proactive use of laxatives can prevent 60 to 70% of severe cases of opioid-induced constipation. The best first-line options are osmotic laxatives like polyethylene glycol (Miralax) and stimulant laxatives like senna or bisacodyl. These work differently: osmotic laxatives pull water into the colon to soften stool, while stimulants gently trigger muscle contractions to move things along.
Don’t just grab any laxative off the shelf. Many people choose stool softeners like docusate, thinking they’re gentle and safe. But research shows they’re often ineffective for OIC. Stick with what works: polyethylene glycol once daily, plus senna if needed. Take them consistently - not just when you feel backed up.
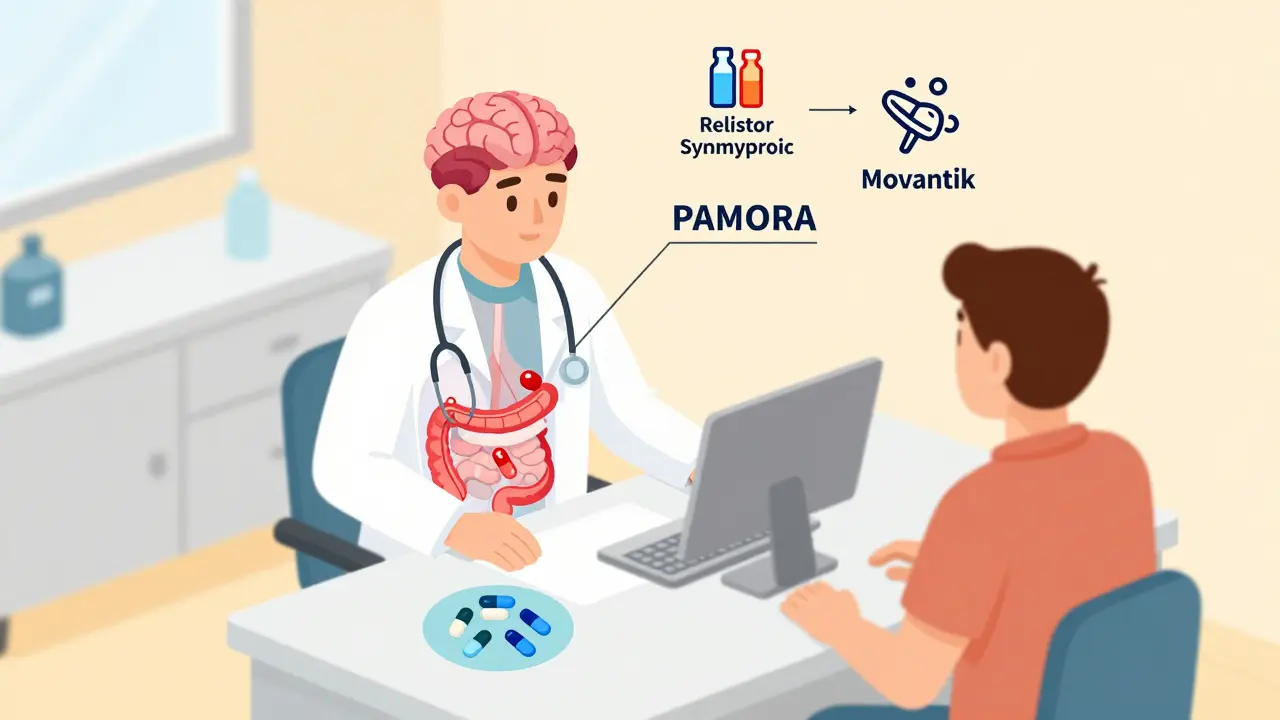
When Laxatives Aren’t Enough: PAMORAs
If you’re on daily laxatives and still struggling, it’s time to talk about PAMORAs - peripherally acting μ-opioid receptor antagonists. These are prescription drugs designed to block opioids in your gut without touching their pain-relieving effects in the brain.There are four main PAMORAs approved for OIC:
- Methylnaltrexone (Relistor®): Given as a subcutaneous injection, it works in about 30 minutes. Often used in palliative care or for patients who can’t swallow pills.
- Naldemedine (Symproic®): A daily oral pill. It’s especially recommended for cancer patients because it may also reduce opioid-induced nausea and vomiting.
- Naloxegol (Movantik®): Another daily pill, taken on an empty stomach. Works well for non-cancer chronic pain.
- Lubiprostone (Amitiza®): Not a PAMORA, but still prescription-only. It activates chloride channels in the gut to increase fluid secretion. Approved for women, but effective in men too.
These aren’t magic bullets. They cost $500 to $900 a month without insurance. Many plans require prior authorization or step therapy - meaning you have to try and fail on cheaper options first. Still, for patients who’ve tried everything else, they’re life-changing. Reddit users and patient forums consistently report: “Relistor works when nothing else does.” “Naldemedine let me stay on my pain meds without constant bathroom struggles.”
Who Should Avoid PAMORAs?
PAMORAs aren’t safe for everyone. They carry a black box warning from the FDA because they can cause gastrointestinal perforation - a serious, potentially fatal tear in the intestinal wall. That risk is higher if you have:- A history of bowel obstruction
- Recent abdominal surgery
- Inflammatory bowel disease (Crohn’s, ulcerative colitis)
- Known or suspected strictures
Doctors also avoid them in patients with severe dehydration or electrolyte imbalances. Always tell your provider about any past GI surgeries or chronic bowel conditions before starting a PAMORA.
Real-World Challenges: Cost, Access, and Patient Hesitation
Even with proven effectiveness, OIC remains under-treated. Why? Three big reasons:- Cost: PAMORAs are expensive. Medicare Part D plans require prior authorization for 41% of prescriptions. Commercial insurers often make patients try and fail on laxatives first.
- Side effects: Nausea, diarrhea, and abdominal pain are common. About 28% of patients on PAMORAs report abdominal discomfort - enough to make some quit.
- Mindset: Many patients don’t want another pill. “I’m already taking five meds,” they say. But the truth is, untreated constipation leads to ER visits, hospitalizations, and worse quality of life.
Pharmacists are stepping in to help. One study showed pharmacist-led education increased appropriate laxative initiation by 43% when opioids were prescribed. That’s huge. If you’re being prescribed an opioid, ask your pharmacist: “Should I start a laxative today?”

Monitoring Progress: The Bowel Function Index
You can’t manage what you don’t measure. The Bowel Function Index (BFI) is a simple 3-question tool doctors use to track OIC severity. It asks about:- Difficulty passing stool
- Feeling of incomplete evacuation
- Straining
A score above 30 means significant constipation that needs treatment change. If you’re on opioids and your BFI is over 30, it’s time to reassess your plan - not just push harder with laxatives.
What’s New in 2026?
The field is evolving fast. In 2023, the FDA approved a once-weekly injectable version of methylnaltrexone, cutting down from daily shots. That’s a big win for patients who struggle with frequent injections.Future developments include oral PAMORAs with better absorption and combo pills that mix low-dose PAMORAs with traditional laxatives. And by 2026, researchers expect to start using genetic testing to predict who responds best to which treatment - meaning less trial and error.
Meanwhile, guidelines are tightening. The American Society of Clinical Oncology now recommends naldemedine as a first-line option for cancer patients starting opioids. The American Society of Gastroenterology is pushing insurers to cover these drugs without barriers, pointing out that untreated OIC costs the U.S. system $2.3 billion a year in avoidable hospital visits.
Bottom Line: Don’t Suffer in Silence
Opioid-induced constipation isn’t a side effect you have to live with. It’s a treatable condition - but only if you act early and know your options. Start a laxative the same day you start your opioid. If that doesn’t work after two weeks, don’t wait. Talk to your doctor about PAMORAs. Keep track of your bowel habits. Use tools like the BFI. And don’t let cost or fear stop you from asking for help.Chronic pain is hard enough. You shouldn’t have to add constant discomfort, embarrassment, or risk of serious complications on top of it. You deserve to manage your pain - and your bowel health - without compromise.
Is opioid-induced constipation the same as regular constipation?
No. Opioid-induced constipation (OIC) is caused by opioids binding to receptors in your gut, which slows movement and hardens stool. Regular constipation is often due to low fiber, dehydration, or inactivity. OIC doesn’t improve with time and doesn’t respond well to standard remedies like fiber supplements or stool softeners alone. It requires targeted treatment, often starting with osmotic laxatives and sometimes needing PAMORAs.
Can I just take more Miralax or senna?
You can start with them - and you should. Polyethylene glycol (Miralax) and senna are first-line treatments. But many patients find that even high doses don’t fully resolve OIC. If you’re taking these daily for more than two weeks and still struggling with straining or incomplete evacuation, it’s time to consider a PAMORA. Don’t keep increasing doses hoping it’ll work - talk to your doctor about next steps.
Do PAMORAs take away my pain relief?
No. PAMORAs are designed to block opioid receptors only in the gut, not in the brain. Their chemical structure prevents them from crossing the blood-brain barrier, so your pain control stays intact. Multiple studies confirm that patients on PAMORAs maintain the same level of pain relief as before. In fact, many report better pain management because they’re no longer distracted by constipation and bloating.
How long does it take for PAMORAs to work?
It depends on the drug. Methylnaltrexone (Relistor®) injections work within 30 minutes. Oral options like naldemedine and naloxegol usually take 24 to 48 hours for the first bowel movement. Most patients see consistent improvement after about a week of daily use. Don’t expect instant results with pills - give them time, but track your response so you know if it’s working.
Is there a cheaper alternative to PAMORAs?
There’s no perfect substitute, but you can try optimizing your current regimen. Use polyethylene glycol daily, add a stimulant like senna if needed, drink plenty of water, and stay active. Some patients find magnesium citrate helpful, though evidence is limited. If you’re still stuck, ask about patient assistance programs - many manufacturers offer discounts or free samples. But if you’ve tried everything and still can’t move your bowels, the cost of untreated OIC - ER visits, hospitalizations, lost work - often outweighs the price of a PAMORA.
Can I stop taking laxatives once I start a PAMORA?
Sometimes, but not always. Many patients continue a low-dose osmotic laxative alongside a PAMORA, especially in the beginning. PAMORAs improve gut motility but don’t always soften stool enough on their own. Your doctor may taper off the laxative after a few weeks if your stools become regular and soft. Never stop or change doses without talking to your provider.
What should I do if I haven’t had a bowel movement in 4 days?
If you’re on opioids and haven’t had a bowel movement in 4 days, don’t wait. Start a stimulant laxative like bisacodyl or senna immediately. If you’re already on a PAMORA, contact your doctor - you may need a suppository or enema. Prolonged constipation can lead to fecal impaction, which requires medical removal. This is not something to manage at home indefinitely. Call your provider or go to urgent care if you’re bloated, nauseated, or in pain.
Are there any natural remedies that work for OIC?
Natural remedies like prune juice, flaxseed, or probiotics might help a little, but they won’t fix opioid-induced constipation on their own. The problem is rooted in how opioids affect your gut nerves - not in diet or microbiome imbalance. Relying on natural options alone can delay effective treatment and lead to complications. Use them as a supplement, not a replacement, for proven medical therapies.


blackbelt security
January 24, 2026 AT 03:40Started Miralax day one with my oxycodone. Still had to switch to Relistor after 3 months. Worth every penny. No more ER visits. No more bloating that made me look 7 months pregnant. Just peace.
Don’t wait. Start early.
Patrick Gornik
January 26, 2026 AT 02:23Let’s be real - this whole OIC discourse is just Big Pharma’s way of monetizing the opioid crisis. You don’t need a $900/month PAMORA. You need to stop taking opioids. The gut isn’t broken - it’s protesting. Your body’s screaming, ‘I didn’t sign up for this!’
Meanwhile, we’re medicating symptoms while ignoring the root cause: dependency masquerading as treatment. Let’s talk about harm reduction, not just laxative escalation.
Also, ‘Miralax’ is just dissolved plastic. You’re not healing - you’re lubricating a sinking ship.
Tommy Sandri
January 26, 2026 AT 04:07While the clinical guidance presented is largely accurate and aligns with current ASCO and ASG recommendations, it is worth noting that access disparities persist across socioeconomic strata. The financial burden of PAMORAs remains a significant barrier, particularly for uninsured and underinsured populations. Community pharmacy initiatives, such as those referenced in the 2024 JAMA Health Forum study, demonstrate measurable improvement in adherence when integrated into primary care workflows. Further policy intervention is required to ensure equitable access to these life-improving therapeutics.
Luke Davidson
January 26, 2026 AT 19:03I was skeptical at first - thought all this PAMORA stuff was just hype
Then I tried naldemedine after 6 months of constipation hell
First day? Nothing
Day 3? I felt like a human again
Now I’m on it with a low-dose Miralax and I can actually sleep through the night without worrying about being backed up
And yeah - my pain didn’t vanish
But I stopped hating my body
That’s worth more than any pill
Karen Conlin
January 28, 2026 AT 09:33To anyone reading this and thinking ‘I’ll just wait and see’ - don’t.
Start the laxative the same day you get the script. No exceptions.
My mom waited three weeks. Ended up in the ER with a fecal impaction. Had to be manually removed.
She cried for days after.
You don’t need to be that person.
Be the one who asks the pharmacist, ‘Should I start something today?’
That’s the difference between suffering and living.
asa MNG
January 29, 2026 AT 00:07ok but like… why do we even have opioids if they turn you into a brick factory? 😭
also i took miralax for 2 years and still felt like i was trying to push a bowling ball outta my butt
then i tried movantik and it was like a miracle… until i got diarrhea and felt like i was in a horror movie
also my insurance denied it 3 times so i had to beg my dr to write a letter and now i’m on it and i still owe $200
but at least i can leave the house without panic
also pls send help
Heather McCubbin
January 29, 2026 AT 20:21So you’re telling me we’ve been gaslighting patients for decades by saying ‘just drink more water’?
And now we’re selling them $900 pills to fix what we created?
Classic. The system doesn’t care if you’re in pain - it cares if you’re profitable.
And don’t even get me started on how doctors act like they’re doing you a favor by even mentioning PAMORAs
They’d rather you suffer than deal with the paperwork
It’s not medicine - it’s corporate theater
Shanta Blank
January 30, 2026 AT 13:12Y’all are missing the point.
This isn’t about laxatives or pills.
This is about the fact that we’ve normalized turning people into walking constipated zombies because ‘they need pain relief’
What if the real solution is not more drugs - but less opioids?
What if we invested in physical therapy, acupuncture, ketamine clinics, nerve blocks - things that don’t turn your colon into a desert?
But no - we’d rather keep prescribing and then slap a $900 bandaid on the wound
And call it progress.
It’s not progress. It’s exploitation dressed in white coats.
Chloe Hadland
February 1, 2026 AT 09:43My dad’s on methylnaltrexone now and he’s finally able to go out to dinner without planning his whole day around the bathroom
He cried when he told me he didn’t have to take senna every night anymore
It’s not glamorous
But it’s real
And it matters
Just… please ask your doctor about this before it’s too late