Statin Dose Adjuster Calculator
Current Statin Details
Switching Strategy
Results & Guidance
Why This Works
LDL Reduction 30-50% with dose adjustment
Side Effect Risk Reduced by 60-80% with proper switching
Cost Most statins are under $50/month
When to Consult Your Doctor
- CK levels >4x upper limit with pain
- Unexplained muscle weakness
- Changes in liver enzymes
Statin medications have saved millions of lives by lowering LDL cholesterol and reducing the risk of heart attacks and strokes. But for some people, the side effects-especially muscle pain-make it hard to keep taking them. If you’ve stopped your statin because of muscle aches, fatigue, or weakness, you’re not alone. And you don’t have to give up on the benefits of statins forever. The key isn’t always quitting the drug-it’s adjusting how you take it.
Why Statin Side Effects Happen
Statin side effects aren’t random. The most common issue is statin-associated muscle symptoms, or SAMS. This includes soreness, stiffness, or weakness in the muscles, usually in the arms, legs, or back. It’s not always serious, but it’s enough to make people stop taking their medication. About 1% to 10% of people report these symptoms, though research shows many of them may not even be caused by the statin itself. A landmark 2023 trial called SAMSON looked at over 6,000 people who thought they couldn’t tolerate statins. The twist? They took both a statin and a placebo-without knowing which was which. The results were surprising: 90% of participants had similar symptoms during both the statin and placebo phases. That suggests a strong nocebo effect. In other words, expecting side effects can make you feel them-even when the drug isn’t the cause. That doesn’t mean muscle pain isn’t real. But it does mean your brain might be playing a role. Still, for those who truly have drug-related muscle issues, the problem often comes down to how the body processes the statin. Some statins are broken down by liver enzymes like CYP3A4. If you’re taking other medications or have certain health conditions, your body might not clear them efficiently. That can lead to higher levels of the drug in your blood, increasing the chance of side effects.When to Consider Dose Adjustment
Before switching statins or stopping altogether, try adjusting the dose. This is often the simplest and most effective first step. Many people can stay on statin therapy with a lower dose or less frequent schedule. For example, if you were taking 40mg of atorvastatin daily and started having muscle pain, your doctor might suggest cutting the dose to 20mg daily-or even 10mg. That’s still enough to lower LDL cholesterol by 30-50%, which is often enough for long-term heart protection. Another option is intermittent dosing. Statins like rosuvastatin and atorvastatin have long half-lives-meaning they stay active in your body for a long time. That makes them perfect for skipping days. You might take your statin every other day, or even just twice a week. Studies show this can still cut LDL by 20-40%, which is a big win for heart health. The American College of Cardiology recommends a minimum two-week break from the statin to confirm symptoms are truly linked to the drug. After that, you can restart at a lower dose or less frequent schedule. For example, starting with rosuvastatin 5mg twice a week, then increasing to three times a week after four weeks if tolerated. This step-by-step approach gives your body time to adjust.Switching Statins: The 75% Solution
If dose changes don’t help, switching to a different statin is the next move-and it works in about 75% of cases. Not all statins are the same. Some are more likely to cause muscle pain than others. Simvastatin, especially at higher doses (40mg or more), has the highest risk. That’s why many doctors avoid it for patients over 65 or those on other medications. Lovastatin is similar. Both are broken down by the CYP3A4 liver enzyme, which means they interact with many common drugs, including some antibiotics, antifungals, and even grapefruit juice. Better alternatives include rosuvastatin (Crestor) and pravastatin (Pravachol). These don’t rely heavily on CYP3A4. Rosuvastatin is especially useful because it’s effective at low doses and has a long half-life, making it ideal for intermittent dosing. Pravastatin is also well-tolerated and doesn’t build up in the body like other statins. One real-world study of over 12,000 statin-intolerant patients found that switching from a CYP3A4-metabolized statin (like simvastatin) to a non-CYP3A4 statin (like rosuvastatin) resolved muscle symptoms in 60-80% of cases. That’s a huge improvement for people who thought they had no options.What About Other Treatments?
If you still can’t tolerate any statin, there are other options-but they come with trade-offs. Ezetimibe (Zetia) is often the first alternative. It lowers LDL by 20-25% by blocking cholesterol absorption in the gut. It’s safe, inexpensive, and works well with low-dose statins. But it doesn’t have the same strong track record for preventing heart attacks as statins do. PCSK9 inhibitors (like Repatha and Praluent) are injectable drugs that cut LDL by 50-70%. They’re powerful. But they cost about $5,800 a year, and most insurance plans require prior authorization. They’re usually reserved for people with very high risk who truly can’t take statins at all. Bile acid resins like cholestyramine can lower LDL by 15-30%, but they often cause bloating, gas, and constipation. Many people can’t stick with them. Some people turn to Coenzyme Q10 supplements, claiming they reduce muscle pain. While it makes sense biologically-statins lower CoQ10 levels-there’s no solid proof from large studies that it helps. A 2021 survey found 58% of users felt better on it, but without controlled trials, we can’t say for sure.
What Else Could Be Causing Your Muscle Pain?
Not every ache is from the statin. Many other things can cause muscle pain, especially in older adults or people with chronic conditions. - Hypothyroidism: Up to 20% of people with statin-related muscle pain also have an underactive thyroid. A simple blood test can check this. - Vitamin D deficiency: Affects 40-60% of the population. Low levels are linked to muscle weakness. Getting your levels checked and correcting them can make a big difference. - Age-related muscle loss: As we get older, we naturally lose muscle mass. That can make any ache feel worse. - Other medications: Blood pressure drugs, antidepressants, and even some antibiotics can interact with statins or cause muscle symptoms on their own. That’s why a good doctor doesn’t just blame the statin. They look at your full picture: your meds, your labs, your lifestyle, and your symptoms.How to Talk to Your Doctor
Don’t just stop your statin and hope for the best. That puts you at higher risk for heart problems. Instead, have a plan. Start by keeping a symptom log. Note when the pain happens, how bad it is, and if anything makes it better or worse. Did it start after you changed your workout routine? After taking a new antibiotic? After skipping sleep? That info helps your doctor figure out if it’s the statin-or something else. Ask your doctor about:- Trying a lower dose
- Switching to rosuvastatin or pravastatin
- Going to every-other-day dosing
- Getting your thyroid and vitamin D levels checked
- Reviewing all your other medications for interactions
The Bigger Picture: Why This Matters
Statin therapy reduces heart attack risk by 25-30% over five years. The number of people you need to treat to prevent one major heart event is just 25. That’s a huge benefit. The risk of serious side effects? Rhabdomyolysis (severe muscle breakdown) happens in fewer than 1 in 1,000 people. Liver damage? Even rarer. For most people, the benefits far outweigh the risks. The goal isn’t to take the highest dose possible. It’s to find the lowest dose that works for you-and stick with it. That’s how you protect your heart for decades.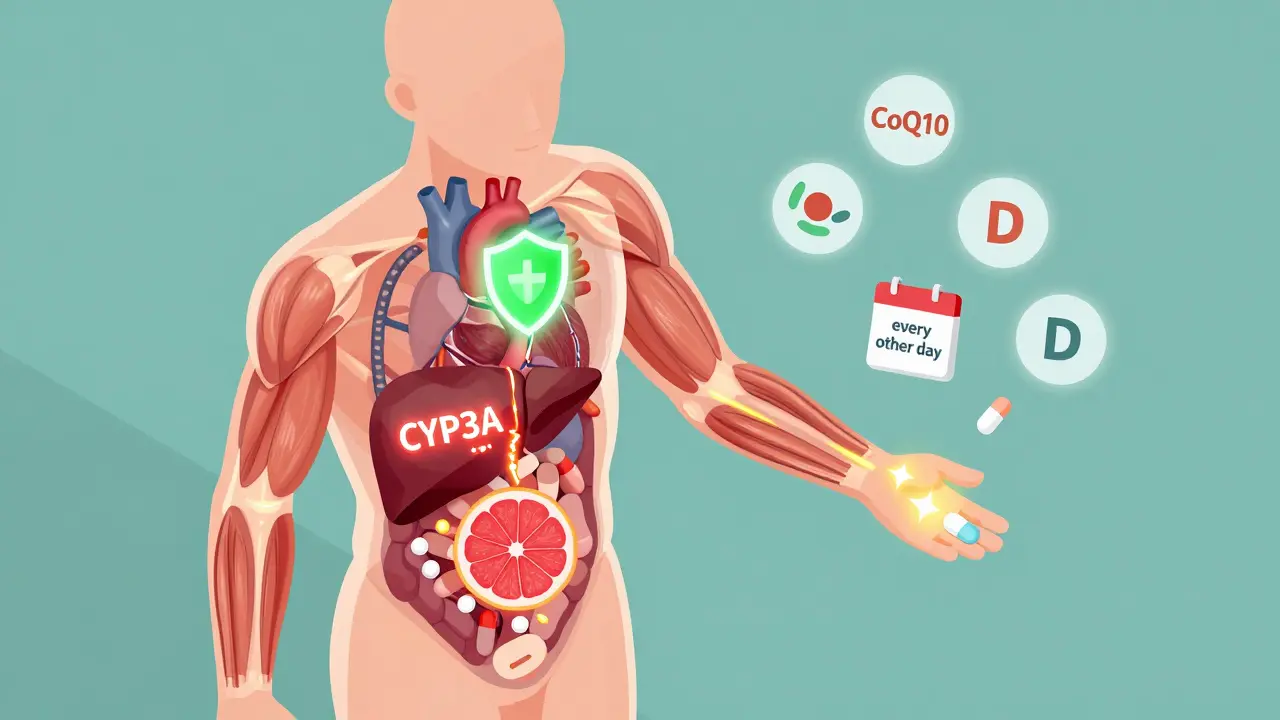
Real Stories: What Works
On patient forums, people share what helped them: - "I switched from simvastatin 40mg to rosuvastatin 10mg every other day. My muscle pain vanished in two weeks. My LDL is now 75. I feel great." - Reddit user, 2023 - "I was on atorvastatin daily and had constant leg cramps. My doctor had me try 5mg rosuvastatin twice a week. No pain. No side effects. I’ve been on it for a year." - AHA Support Network, 2023 - "I tried CoQ10, vitamin D, and stretching. Nothing helped until I switched from simvastatin to pravastatin. Game-changer." - Patient.info survey, 2022 These aren’t outliers. They’re examples of what happens when you don’t give up on statins-you just change how you take them.What to Avoid
- Don’t quit cold turkey. Your cholesterol will rise fast. - Don’t assume all muscle pain is from statins. Get tested for other causes. - Don’t take high-dose simvastatin if you’re over 65 or on other medications. - Don’t rely on supplements without evidence. CoQ10 might help, but it’s not a replacement for proper dosing. - Don’t skip follow-up blood tests. Your doctor needs to check your liver enzymes and CK levels after a dose change.Final Takeaway
Statin side effects are frustrating, but they’re rarely a dead end. You don’t have to choose between heart health and feeling well. With smart dose adjustments, smart switching, and careful monitoring, most people can find a regimen that works. The key is to work with your doctor-not against them. Statins are one of the most studied and effective drugs ever made. Don’t let side effects rob you of their benefits. Adjust. Switch. Try again. Your heart will thank you.Can I take statins every other day instead of daily?
Yes, for certain statins like rosuvastatin and atorvastatin, every-other-day dosing is a proven strategy. These statins have long half-lives (19 and 14 hours, respectively), so they remain active in your bloodstream for days. Studies show this approach can lower LDL by 20-40%, which is enough for most people. It also reduces side effects. Start with a lower dose (like 5mg every other day) and monitor your cholesterol and symptoms over 4-6 weeks.
Why do some statins cause more muscle pain than others?
It comes down to how your body processes them. Statins like simvastatin and lovastatin are broken down by the CYP3A4 liver enzyme. Many common medications, supplements, and even grapefruit juice block this enzyme. That causes the statin to build up in your blood, increasing muscle pain risk. Rosuvastatin and pravastatin use different pathways, so they’re less likely to interact and cause side effects. That’s why switching to one of these often resolves the problem.
Is it safe to stop statins if I have muscle pain?
Not without a plan. Stopping statins suddenly raises your LDL cholesterol within weeks, increasing your risk of heart attack or stroke. If you have muscle pain, don’t quit. Talk to your doctor first. A two-week break to confirm symptoms are statin-related, followed by a switch to a different statin or lower dose, is the safest approach. Most people can return to statin therapy successfully with the right adjustment.
What’s the best statin for people with muscle pain?
Rosuvastatin (Crestor) is often the best choice. It’s not metabolized by CYP3A4, so it has fewer drug interactions. It’s also effective at low doses (5mg or 10mg) and works well with intermittent dosing. Pravastatin is another good option, especially for older adults or those with kidney issues. Both have better safety profiles than simvastatin or lovastatin, which are linked to higher muscle pain rates.
Can I take CoQ10 to prevent statin side effects?
Some people report feeling better when they take CoQ10 supplements (200mg daily), and it makes biological sense-statins lower CoQ10 levels in muscles. But large, well-controlled studies haven’t proven it works. A 2021 survey found 58% of users felt improvement, but without a placebo group, we can’t rule out the placebo effect. It’s safe to try, but don’t rely on it. Dose adjustment or switching statins is far more reliable.
How long should I wait before trying a statin again after stopping?
Wait at least two weeks after stopping the statin to make sure your muscle pain has fully resolved. Then, restart with a different statin or lower dose. For example, if you had pain on simvastatin, try rosuvastatin 5mg twice a week. Monitor symptoms and get a blood test for creatine kinase (CK) after four weeks. If symptoms return, stop again and talk to your doctor about other options.
Do I need blood tests if I’m adjusting my statin dose?
Yes. Your doctor should check your liver enzymes and creatine kinase (CK) before and about four weeks after a dose change or switch. CK levels above four times the upper limit of normal with muscle pain mean you should stop the statin for at least six weeks. Even if you feel fine, these tests catch early signs of muscle damage before it becomes serious.
Can I take ezetimibe instead of a statin?
Ezetimibe is a good option if you truly can’t take any statin. It lowers LDL by 20-25% and is safe for long-term use. But it doesn’t have the same heart-protective track record as statins. Studies show statins reduce heart attacks and strokes more reliably. Many doctors combine ezetimibe with a low-dose statin for better results. Only use it alone if statins are completely intolerable.


Neha Motiwala
February 13, 2026 AT 17:43Gloria Ricky
February 14, 2026 AT 17:45Luke Trouten
February 15, 2026 AT 15:06Kristin Jarecki
February 15, 2026 AT 18:21Jonathan Noe
February 15, 2026 AT 21:38Jim Johnson
February 16, 2026 AT 10:55Vamsi Krishna
February 16, 2026 AT 19:39Brad Ralph
February 18, 2026 AT 03:59