When your parathyroid glands don’t make enough hormone, your body can’t keep calcium in balance. That’s hypoparathyroidism - a rare but serious condition that leaves you with low calcium, high phosphate, and a constant need to manage your diet, pills, and symptoms. It’s not something you recover from. It’s something you learn to live with - day after day.
Why Your Body Can’t Hold Onto Calcium
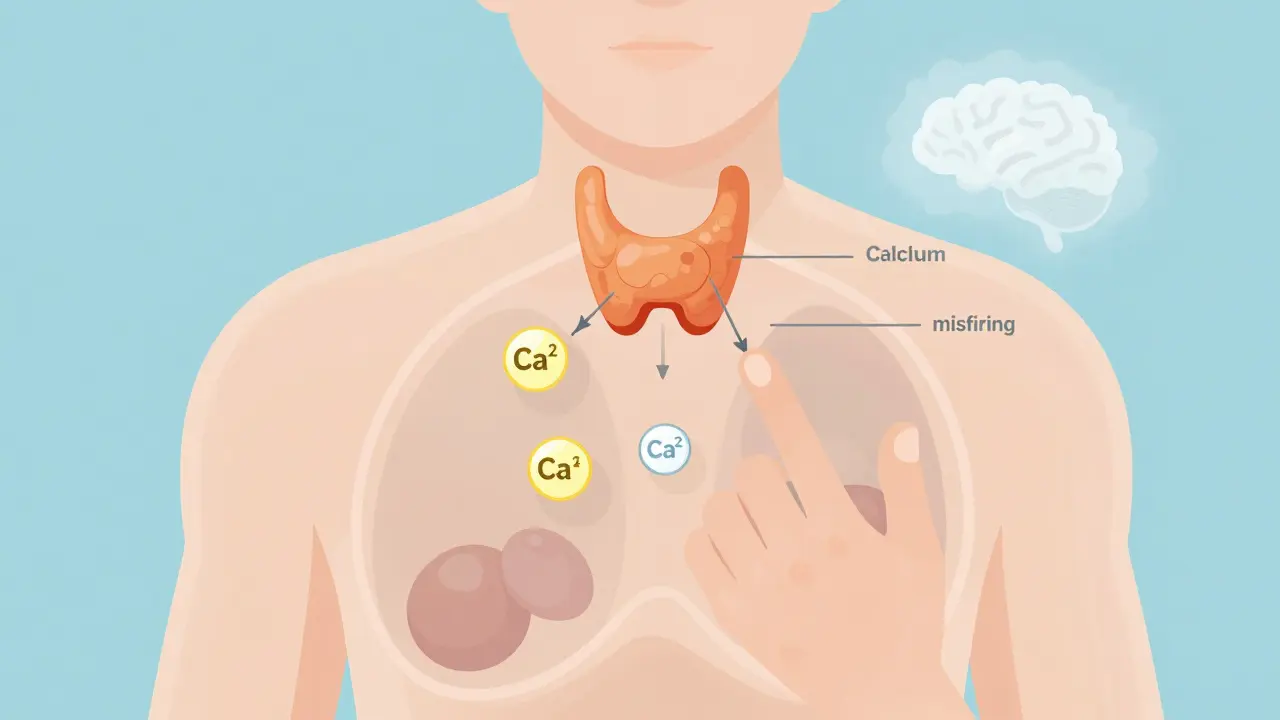
Your parathyroid glands, four tiny nodes behind your thyroid, are responsible for one thing: keeping calcium levels steady. When they’re damaged - often after thyroid surgery - they stop working. No PTH means your kidneys can’t hold onto calcium, your bones don’t release it properly, and your gut can’t absorb it from food. The result? Low blood calcium. You might feel it in your fingers: tingling, numbness, muscle cramps. Or in your heart: irregular beats. Or in your brain: brain fog, anxiety, fatigue.
Most cases happen after neck surgery. About 8 out of 10 people with hypoparathyroidism got it after a thyroidectomy. But it can also come from autoimmune disease, genetics like DiGeorge syndrome, or radiation. No matter the cause, the outcome is the same: your body needs help to replace what it can’t make.
The Standard Treatment: Calcium and Active Vitamin D
There’s no cure. So treatment focuses on replacing what’s missing. The standard approach? Calcium supplements and active vitamin D - not regular vitamin D3, but calcitriol or alfacalcidol. Why? Because your body can’t convert regular vitamin D into its active form without PTH. Calcitriol skips that step. It works directly.
Doctors typically start with 1,000 to 2,000 mg of calcium daily, split into two or three doses. Take it with meals. That’s not just for absorption - it also helps bind phosphate in your gut, keeping levels down. The best form? Calcium carbonate. It gives you 40% elemental calcium. So if you need 1,000 mg of elemental calcium, you take 2,500 mg of calcium carbonate. Calcium citrate? Only 21%. You’d need way more pills.
For active vitamin D, the starting dose is usually 0.25 to 0.5 mcg of calcitriol per day. Some people need more. Some need less. But the goal isn’t to push calcium into the normal range. It’s to keep it in the lower half - between 2.00 and 2.25 mmol/L (or 8.0 to 8.5 mg/dL). Why? Because going higher increases your risk of kidney stones, calcium deposits in your brain, and long-term kidney damage.
What You Must Monitor - And Why
Treatment isn’t set-and-forget. You need regular blood and urine tests. Every 1 to 3 months at first. Then, if things stabilize, maybe twice a year.
- Serum calcium: Keep it between 2.00-2.25 mmol/L. Higher than that? You’re risking calcification in your kidneys, brain, or blood vessels.
- 24-hour urinary calcium: This is critical. You want less than 250 mg per day. More than that? You’re flushing calcium out and increasing kidney stone risk by 5 to 7 times. Many patients don’t realize this test is needed before any dose increase.
- Serum phosphate: Should be 2.5-4.5 mg/dL. Too high? You get itching, bone pain, and vascular calcification. Too low? Muscle weakness. It’s a tight rope.
- Magnesium: Below 1.7 mg/dL? Your body can’t use PTH even if it’s there. Supplement with magnesium oxide or citrate - 400-800 mg daily if needed.
- 25-hydroxyvitamin D: Keep it between 20-30 ng/mL. That’s why you still take 400-800 IU of vitamin D3 daily, even on active D analogues.
One mistake patients make? Skipping the urine test. They see their blood calcium is “normal” and think they’re fine. But if their urine calcium is 400 mg/day, they’re quietly damaging their kidneys. That’s why the 2022 JBMR guidelines say: never increase doses without checking urine calcium first.
Diet: What to Eat - and What to Avoid
You can’t just rely on pills. Food matters.
Get calcium from dairy: one cup of milk = 300 mg. One serving of yogurt = 250-300 mg. Leafy greens like kale (100 mg per cup) and broccoli (43 mg per cup) help too. But don’t count on spinach - it has oxalates that block calcium absorption.
Now, the hard part: cutting phosphorus. Processed foods are loaded with it. Soda? One liter of cola has 500 mg of phosphoric acid. Processed meats? 150-300 mg per serving. Hard cheese? 500 mg per ounce. Even some breads and cereals have added phosphates.
Stick to whole foods: fresh meat, vegetables, fruits, plain rice, oats. Avoid anything with “phos” on the ingredient list. That’s phosphate additive - not natural. And it’s absorbed almost 100% by your body, unlike natural phosphorus in food.
Also, limit salt. Sodium makes your kidneys dump calcium. Keep sodium under 2,000 mg per day. That means no processed snacks, canned soups, or fast food.
When the Standard Treatment Isn’t Enough
About 25-30% of people with hypoparathyroidism can’t get stable with calcium and vitamin D alone. They need too much - more than 2 grams of calcium or 2 mcg of calcitriol daily. They still have symptoms. Their urine calcium stays high. Their quality of life tanks.
That’s when doctors consider PTH replacement. Two options exist: Natpara (recombinant human PTH 1-84) and Forteo (teriparatide, a fragment of PTH). Natpara is approved for hypoparathyroidism. Forteo is technically for osteoporosis, but some doctors use it off-label.
Here’s the catch: Natpara costs about $15,000 a month. Conventional therapy? $100-200. Natpara requires a daily injection. You need a special pharmacy. You need a REMS program enrollment - a safety system because of a small risk of bone cancer in animal studies. Many patients wait 30-45 days just to get it approved.
But for some, it’s life-changing. A 2019 study showed patients on PTH therapy cut their calcium and vitamin D needs by 30-40%. They had fewer symptoms. Better sleep. More energy. One patient in the Hypopara Registry said, “I went from 8 pills a day to 3. I finally feel like myself.”
What Works in Real Life - Patient Tips
Real people with hypoparathyroidism have figured out tricks that help.
- Split your calcium doses. Instead of 3 pills twice a day, try 2 pills 4-5 times a day. Smaller doses = better absorption. Less stomach upset. Less constipation.
- Take vitamin D at bedtime. It’s fat-soluble. Taking it with your last meal helps absorption.
- Track your symptoms. Keep a log: tingling? Cramps? Fatigue? When did you take your pills? What did you eat? Patterns emerge. You’ll see that pizza at 7 PM causes cramps at 11 PM.
- Don’t skip magnesium. If you’re tired and crampy even with good calcium levels, check your magnesium. Many doctors forget this.
- Have an emergency plan. If you feel sudden numbness, tingling, or a seizure coming on - chew 2-3 calcium tablets right away. Call your doctor. Go to the ER if it doesn’t improve.
Reddit’s r/Hypoparathyroidism community has over 1,200 members. The top post? “How I stopped the calcium rollercoaster.” People share how they fixed their schedule, found a good endocrinologist, or got insurance to cover Natpara. It’s not just information - it’s survival tips.

What’s Coming Next
Science is moving fast. TransCon PTH, a once-daily long-acting PTH injection, showed in a 2022 trial that 89% of patients could normalize calcium without calcium supplements. It’s not approved yet, but Phase 3 results are promising. If it gets through, it could replace daily pills for many.
Gene therapy is in early animal studies. Targeting the calcium-sensing receptor could one day fix the body’s ability to detect calcium levels - no injections, no pills. But human trials? Not before 2026.
Right now, the biggest risk isn’t low calcium. It’s long-term damage from over-treatment. A 2022 Cleveland Clinic study found that patients with calcium levels above 2.35 mmol/L for more than 15 years had nearly 3 times the risk of calcium deposits in their brain. That’s why doctors now say: aim lower, not higher.
Who Manages This? And How Often?
You need an endocrinologist - not your GP. Most family doctors say they feel untrained in this. Only 22% feel confident managing hypoparathyroidism, according to a 2021 AAFP survey.
Start with 3-4 visits in the first 3 months. Then, once stable, 3-4 visits a year. But if you’re on PTH therapy, you’ll need more. Blood tests every 4-6 weeks at first. Urine tests every 3 months.
Keep a binder. Or a phone app. Write down your doses, your symptoms, your lab results. Bring it to every appointment. You’re the expert on your body. Your doctor is the expert on the science. Together, you make the plan.
Can you cure hypoparathyroidism?
No, there is no cure. Hypoparathyroidism is a lifelong condition. Treatment focuses on replacing what your body can’t produce - calcium and active vitamin D - to keep symptoms under control and prevent complications. New therapies like TransCon PTH may reduce pill burden, but they don’t restore natural hormone production.
Why is active vitamin D used instead of regular vitamin D3?
Your body needs parathyroid hormone (PTH) to convert regular vitamin D (cholecalciferol) into its active form. With hypoparathyroidism, that conversion doesn’t happen. Active vitamin D analogues like calcitriol are already activated, so they bypass the missing step. Studies show calcitriol works 2.3 times faster than D3 at raising calcium levels.
Is it safe to take calcium supplements long-term?
Yes - if you’re monitored. The risk isn’t calcium itself, but too much calcium in your urine. That leads to kidney stones and long-term kidney damage. The key is keeping urinary calcium under 250 mg/day. Take calcium with meals, avoid excess doses, and get regular urine tests. Avoid calcium doses over 2,000 mg elemental calcium daily unless absolutely necessary.
Can low magnesium cause low calcium in hypoparathyroidism?
Yes. Even if your parathyroid glands are damaged, your body still needs magnesium to use any remaining PTH - or to respond to calcium supplements. If magnesium drops below 1.7 mg/dL, calcium levels won’t stabilize. That’s why doctors check it routinely and often prescribe magnesium supplements alongside calcium and vitamin D.
What should I do if I miss a dose of calcium or vitamin D?
If you miss one dose, take it as soon as you remember - but don’t double up. If you miss more than one dose and feel tingling, cramps, or anxiety, chew 2-3 calcium tablets immediately. Call your doctor. Don’t wait. Symptoms can escalate quickly. Keep emergency calcium tablets in your bag, car, and desk.
Can I stop taking calcium if my levels look normal?
Never stop without medical supervision. Even if your blood calcium looks normal, your body still can’t make PTH. Stopping treatment will cause levels to drop - sometimes within hours. Symptoms can return suddenly. Hypocalcemia can trigger seizures or heart rhythm problems. This is not a condition you can manage by feel.
Final Thoughts: Balance Is Everything
Hypoparathyroidism isn’t about fixing a number. It’s about finding a rhythm - between pills and meals, between symptoms and stability, between caution and living. It’s exhausting. It’s complicated. But it’s manageable.
Most people who stick with the plan - tracking their labs, eating clean, splitting doses, checking magnesium - live full lives. They work. They travel. They raise kids. They don’t let the condition define them.
The goal isn’t perfection. It’s control. And with the right approach, you can have both.

James Rayner
December 16, 2025 AT 15:02Just wanted to say this post is one of the most thorough, compassionate summaries I’ve ever read on hypoparathyroidism. Seriously. You didn’t just list facts-you showed the human rhythm behind the numbers. 🙏
Kim Hines
December 16, 2025 AT 20:12I’ve had this for 11 years. Still can’t believe how many doctors don’t know about the urine calcium test.
Kitty Price
December 17, 2025 AT 14:04This is exactly what I needed to show my endo. I’ve been begging them to check my urinary calcium for months. Finally, someone explains why it matters.
Cassandra Collins
December 18, 2025 AT 17:41Wait… so Natpara is expensive because Big Pharma is holding it hostage? I bet they’re also hiding the fact that it causes brain tumors. They did the same with insulin. You think they really care about you? 🤔
sue spark
December 20, 2025 AT 11:27Splitting calcium doses changed my life. I used to feel like a zombie by noon. Now I’m actually awake. Also magnesium is non negotiable. I wish more doctors said that.
Mike Smith
December 21, 2025 AT 22:53Thank you for writing this with such precision and heart. The emphasis on urinary calcium monitoring is critical-and far too often overlooked. I’ve seen patients develop nephrocalcinosis because they were told ‘your blood calcium is fine’ and never tested urine. This is the kind of guidance that saves kidneys-and lives.
Also, the point about magnesium is spot on. I’ve had patients with perfectly normal calcium and phosphate levels who still had severe cramping-until we checked magnesium. It’s not an afterthought. It’s a cornerstone.
And to those considering PTH replacement: yes, the cost is brutal, yes, the bureaucracy is a nightmare-but for many, it’s the difference between surviving and thriving. The data is clear. Quality of life improves. Symptom burden drops. Don’t let insurance gatekeeping silence your need.
Keep advocating. Keep tracking. Keep sharing. This community is stronger because of posts like this.
SHAMSHEER SHAIKH
December 22, 2025 AT 13:02As a physician practicing in Mumbai, I have encountered several cases of post-thyroidectomy hypoparathyroidism, and I must say, this article is one of the most meticulously structured, evidence-based, and patient-centered summaries I have ever encountered. The distinction between calcium carbonate and citrate, the emphasis on urinary calcium excretion, the warning against phosphate additives-all of these are critical, yet routinely neglected in clinical practice. I have shared this with my residents and patients alike. The inclusion of real-life tips-such as taking vitamin D at bedtime and splitting doses-is not merely practical; it is transformative. Moreover, the mention of TransCon PTH as a future standard is both hopeful and scientifically grounded. The challenge remains: how do we ensure that such knowledge reaches not only the well-resourced but also those in resource-limited settings? Perhaps open-access platforms like this can bridge that gap.
Additionally, I would add that many patients in India are prescribed generic calcitriol, which is affordable and effective-but often without proper guidance on timing or dietary phosphorus control. The dietary advice here-avoiding ‘phos’ on labels-is invaluable. I urge all clinicians to distribute this as a handout. This is not just information; it is empowerment.
Dylan Smith
December 23, 2025 AT 07:42My husband was diagnosed after thyroid surgery and we’ve been fighting insurance for Natpara for 14 months. They denied it three times. We appealed. Got a letter from our endo. Got a letter from a patient advocacy group. Finally approved last month. We’re on it now. The difference? Night and day. No more midnight cramps. No more brain fog. I can’t believe how long we waited because of bureaucracy. This isn’t a luxury. It’s medicine. And if you’re on the fence about applying-do it. Even if they say no. Keep going. You’re worth it.
Colleen Bigelow
December 24, 2025 AT 18:43They want you to believe this is just a hormone problem but it’s not. It’s a control experiment. They don’t want you cured because then you’d stop buying pills. They don’t want you on Natpara because it’s too cheap to produce. The real cure? A pill that makes your body produce PTH again? Nah. That’d kill the market. They’d rather you take 10 pills a day for life and get kidney stones. Look at the stats. 8 out of 10 cases come from thyroid surgery. Coincidence? Or is it a business model? They cut your glands, then sell you the fix. And they profit from your suffering. Don’t fall for it.