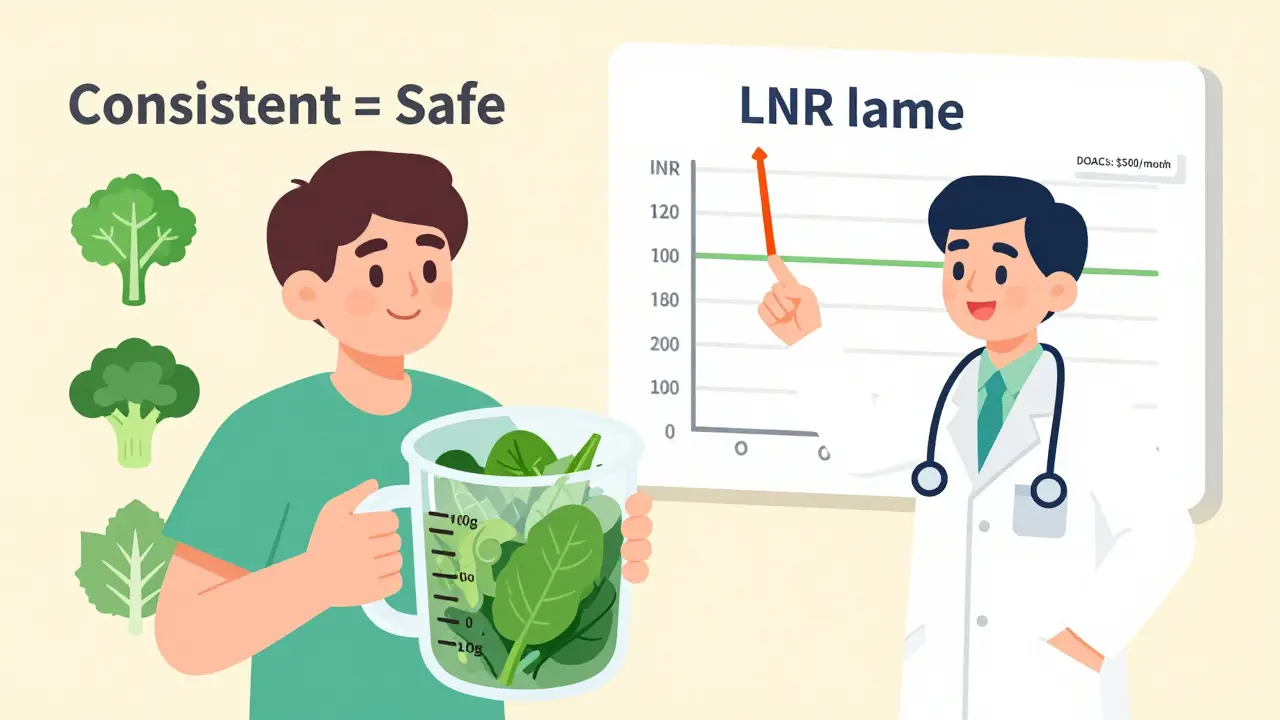
When you're on warfarin, the last thing you want is a surprise in your bloodwork. That spike in INR? The sudden drop? More often than not, it’s not the medication failing-it’s your greens. But here’s the truth most people don’t tell you: you don’t need to give up spinach, kale, or broccoli. You just need to keep eating them the same way, every day.
Why Warfarin and Leafy Greens Don’t Mix-At First Glance
Warfarin works by blocking vitamin K, a nutrient your body needs to make clotting proteins. If you eat more vitamin K, warfarin loses some of its punch. Eat less, and your blood thins too much. That’s why doctors used to tell patients: avoid greens. But that advice was wrong. The real problem isn’t vitamin K. It’s inconsistency. One day you eat a big salad. The next, you skip it. Your INR swings like a pendulum. That’s when clots form-or you start bleeding internally. The data doesn’t lie: 38% of warfarin-related ER visits in 2021 were tied to sudden changes in vitamin K intake, according to the American Heart Association.What Counts as a High-Vitamin K Food?
Not all greens are equal. Some pack a serious punch:- Cooked spinach: 889 mcg per cup
- Cooked kale: 547 mcg per cup
- Cooked collard greens: 772 mcg per cup
- Cooked broccoli: 220 mcg per cup
- Cooked cabbage: 415 mcg per cup
The Science Behind Consistency
A 2024 study from Universitas Padjadjaran, published by the NIH, followed warfarin patients who ate exactly 100 grams of spinach daily. That’s about one cup cooked. After eight weeks, their INR levels didn’t just stay stable-they improved. No bleeding, no clots. Just steady results. This isn’t an outlier. It’s the rule. The American College of Chest Physicians (CHEST 2021 Guidelines) says it clearly: “We suggest that patients receiving vitamin K antagonists maintain a consistent intake of vitamin K rather than avoiding vitamin K-rich foods.” The evidence? Solid. The recommendation? Conditional, but backed by decades of real-world use. Doctors at Brigham and Women’s Hospital put it simply: “Keep it consistent from week to week.” Minor day-to-day changes? Fine. Big swings? Dangerous.What Happens When You Flip the Script?
If you suddenly eat twice as many greens:- Your INR can drop by 0.5-1.0 in 3-5 days
- Your blood thickens
- You’re at higher risk for stroke or pulmonary embolism
- Your INR can jump up by the same amount
- Your blood thins too much
- You risk bleeding in the brain, gut, or joints

What Can You Eat Without Worrying?
You don’t have to live on white rice and chicken breast. There are plenty of low-vitamin K vegetables you can eat freely:- Lettuce (½ cup / 80g)
- Carrots (3 dessert spoons)
- Cauliflower (8 florets)
- Courgettes (½ large one)
- Mushrooms (3-4 dessert spoons)
- Green beans
- Potatoes
- Onions
What About Newer Blood Thinners?
Yes, there are alternatives: apixaban (Eliquis), rivaroxaban (Xarelto), dabigatran (Pradaxa). These DOACs don’t care about vitamin K. You can eat kale smoothies and not worry. But here’s the catch: they cost $500-$600 a month. Warfarin? $4-$10. For millions of people, especially those without good insurance, warfarin is the only option. And it’s not just about money. Warfarin is still the only choice for people with mechanical heart valves-especially in the mitral position. DOACs are banned here. No exceptions. So if you’re on warfarin, you’re not stuck with outdated care. You’re on a proven, affordable, and effective treatment. You just need to learn how to eat with it.Practical Tips for Daily Life
Here’s how to make this work without stress:- Choose one high-vitamin K food you like (spinach, kale, broccoli). Stick to it.
- Measure it. Use a kitchen scale or measuring cup. 100g of spinach? That’s one cup cooked. Make it your daily standard.
- If you want to change your greens? Talk to your doctor first. Don’t swap kale for collards on a whim.
- Keep a simple food log. Just write down what you ate and how much. No apps needed-pen and paper works.
- Don’t take supplements like St. John’s Wort, Ginkgo Biloba, or cod liver oil. They interfere with warfarin too.
- If you get sick-diarrhea, fever, vomiting-call your clinic. Your body absorbs vitamin K differently when you’re ill.
What About Juice, Smoothies, and Supplements?
Green smoothies? If you make one with a whole bunch of kale and spinach, and you didn’t do that yesterday? That’s a problem. Same with bottled kale juice. One bottle could be 500 mcg of vitamin K. That’s more than half your weekly dose in one drink. If you love smoothies, stick to low-K ingredients: banana, berries, carrots, yogurt. Add one handful of spinach, and keep it the same every time. And no, you can’t “catch up” on vitamin K. If you skip your greens for three days and then eat three cups on day four? That’s a recipe for an INR crash.What About Other Foods and Drinks?
Grapefruit juice? Avoid it. It changes how your liver breaks down warfarin. Alcohol? Keep it moderate. More than two drinks a day can raise your INR. Garlic and ginger? Fine in food amounts. But don’t start taking garlic pills. They thin your blood too. And don’t forget: some antibiotics can boost vitamin K levels. If you’re prescribed one, tell your doctor you’re on warfarin. They’ll need to check your INR sooner.The Bottom Line
You don’t have to give up your greens to stay safe on warfarin. You just have to be predictable. Eat the same amount of vitamin K-rich food every day. Keep your INR steady. Avoid the ER. Save money. Stay healthy. This isn’t about restriction. It’s about control. You’re not a patient who needs to follow rules-you’re someone who knows how to manage their health. And that’s powerful.Can I eat spinach if I’m on warfarin?
Yes, you can eat spinach on warfarin-but only if you eat the same amount every day. A 2024 NIH study found that 100 grams (about one cup cooked) of spinach daily is safe and helps keep INR levels stable. Sudden changes in intake, not the spinach itself, are what cause problems.
What happens if I eat more leafy greens one day?
Eating more vitamin K-rich foods in one day can lower your INR within 3-5 days, making your blood less likely to clot. This raises your risk of stroke or blood clots. If you accidentally eat a big serving, don’t panic-but tell your doctor. They may need to check your INR sooner.
Is kale better than spinach for warfarin users?
Neither is better. Kale has slightly less vitamin K than spinach (547 mcg vs. 889 mcg per cup cooked), but both are high. The key isn’t which green you pick-it’s consistency. Pick one and stick to it. Swapping kale for spinach daily can cause dangerous INR swings.
Do I need to avoid all vegetables on warfarin?
No. Only high-vitamin K vegetables need attention. You can eat unlimited amounts of carrots, lettuce, mushrooms, potatoes, onions, green beans, and cauliflower. These are low in vitamin K and won’t interfere with your medication.
Why do some doctors still say to avoid greens?
Some older advice still circulates, but it’s outdated. Major medical groups like the American College of Chest Physicians, Mayo Clinic, and NHS now all agree: consistency over avoidance. Avoiding greens can lead to low vitamin K levels, which actually increases bleeding risk. The goal is balance-not elimination.
Can I switch to a newer blood thinner to avoid this?
Yes, newer anticoagulants like Eliquis and Xarelto don’t interact with vitamin K. But they cost 50-100 times more than warfarin and aren’t safe for everyone-especially people with mechanical heart valves. For many, warfarin remains the best option, and with consistent eating, it works very well.
How often should I get my INR checked?
If your diet is stable, you’ll usually get checked every 4-6 weeks. But if you’ve changed your food habits, had an illness, or started a new medication, your doctor may want to check it weekly until your levels stabilize. Always tell your provider about any dietary changes.
What supplements should I avoid with warfarin?
Avoid St. John’s Wort, Ginkgo Biloba, Danshen, glucosamine, and cod liver oil. These can interfere with warfarin’s effects or increase bleeding risk. Even “natural” supplements aren’t safe. Always check with your doctor before taking anything new.


Jarrod Flesch
January 21, 2026 AT 00:30michelle Brownsea
January 21, 2026 AT 20:25Sangeeta Isaac
January 22, 2026 AT 14:26Gerard Jordan
January 23, 2026 AT 12:11Melanie Pearson
January 25, 2026 AT 07:37Stephen Rock
January 25, 2026 AT 19:37Kelly McRainey Moore
January 26, 2026 AT 23:54lokesh prasanth
January 28, 2026 AT 23:33Andrew Rinaldi
January 30, 2026 AT 21:12Uju Megafu
February 1, 2026 AT 00:19Roisin Kelly
February 2, 2026 AT 07:58Philip Williams
February 3, 2026 AT 18:55Ashok Sakra
February 4, 2026 AT 15:12