Kidney Risk Calculator
This calculator estimates your risk of drug-induced kidney injury based on the article's clinical guidelines. Input your details to get personalized recommendations.
What Is Drug-Induced Kidney Failure?
Drug-induced kidney failure, more accurately called drug-induced acute kidney injury (DI-AKI), happens when certain medications suddenly damage your kidneys. It’s not a slow, inevitable decline-it’s a sharp drop in kidney function that can occur within hours or days after taking a drug. This isn’t rare. About 1 in 5 cases of acute kidney injury in hospitals comes from medications. In intensive care units, that number jumps to 30-60%.
The kidneys filter waste, balance fluids, and regulate blood pressure. When drugs interfere with those jobs, things go wrong fast. Some medications cause inflammation in the kidney tissue. Others form crystals that block tiny tubes inside the kidneys. Some reduce blood flow, starving the kidneys of oxygen. The damage can be reversible-if caught early. But if ignored, it can lead to permanent scarring, dialysis, or even death.
How Do You Know It’s Happening?
There’s no single symptom that screams "kidney damage from drugs." That’s why so many cases are missed. People often feel fine until it’s too late. But here’s what to watch for:
- A sudden drop in urine output-less than half a cup per hour for six hours or more
- Swelling in the ankles, legs, or face
- Unexplained fatigue, nausea, or confusion
- Back pain just below the ribs
- Fever or rash, especially if you’ve started a new antibiotic or painkiller in the past week
These signs are often mistaken for other problems. A fever might be blamed on an infection. Swelling might be chalked up to eating too much salt. But if you’ve recently started a new medication and notice any of these, get your creatinine checked. A rise of just 0.3 mg/dL in two days is a red flag.
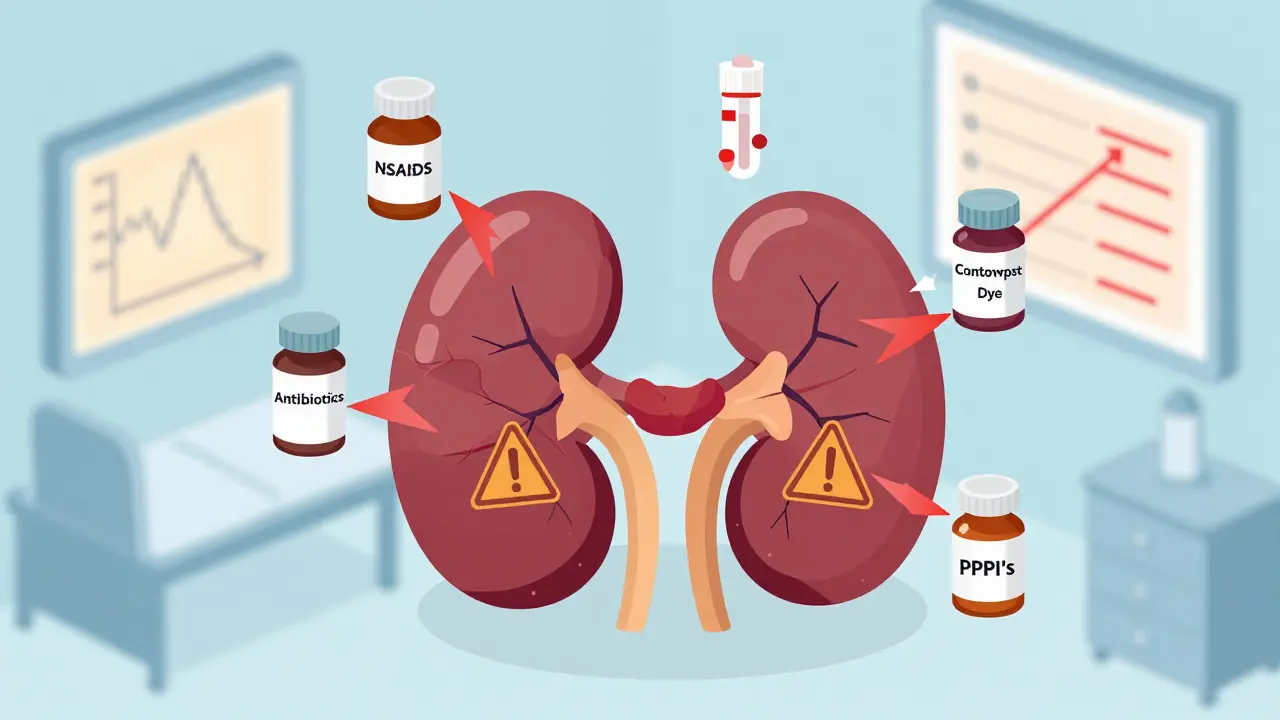
Top Medications That Hurt Your Kidneys
Not all drugs are equally dangerous. Some are common, widely used, and quietly damaging. Here are the biggest culprits:
- NSAIDs (ibuprofen, naproxen, diclofenac): These over-the-counter painkillers are responsible for 3-5% of all hospital kidney injuries. For someone over 65 or with existing kidney trouble, the risk jumps to 15-20%. A single week of daily use can crash kidney function in vulnerable people.
- Antibiotics (vancomycin, piperacillin-tazobactam, sulfonamides): Vancomycin alone causes 2.7 cases per 1,000 patient-years. Sulfonamides (like Bactrim) can trigger crystal buildup in the kidneys unless urine is kept alkaline (pH above 7.1) and you drink at least 3 liters of water daily.
- Proton pump inhibitors (omeprazole, pantoprazole): Used for heartburn, these are now linked to acute interstitial nephritis-a type of kidney inflammation that shows up weeks after starting the drug.
- Contrast dye (used in CT scans): Causes about 10% of hospital-acquired kidney injuries. Risk is highest in diabetics, older adults, and those already with reduced kidney function.
- Chemotherapy and antivirals (acyclovir, tenofovir): Acyclovir forms crystals in the urine. Tenofovir slowly damages kidney tubules over time, especially if used with other nephrotoxic drugs.
Here’s the hard truth: You don’t need to be on a dangerous drug for long to get hurt. One study found that 40% of DI-AKI cases happened within the first 3 days of starting the medication.
Who’s at Highest Risk?
It’s not just the elderly or the chronically ill. But certain people are far more vulnerable:
- People with eGFR below 60 (signs of chronic kidney disease)
- Those taking five or more medications daily (polypharmacy increases risk 3.7 times)
- Patients with diabetes or heart failure (reduced blood flow to kidneys)
- Older adults over 70
- People who are dehydrated or on diuretics
What’s worse? Many of these people are never screened. A 2019 audit found that 31% of patients admitted to the hospital with kidney injury had no baseline creatinine test before starting risky meds. That’s like driving blindfolded.
How to Prevent It-Step by Step
Here’s the good news: 60-70% of drug-induced kidney injuries are preventable. You don’t need fancy tech or expensive tests. Just a few smart moves.
- Know your baseline: Before starting any new medication-especially NSAIDs, antibiotics, or contrast dye-ask for a simple blood test to check your creatinine and calculate your eGFR. If your eGFR is below 60, your doctor should adjust your doses or avoid certain drugs entirely.
- Avoid NSAIDs if you have kidney issues: If you’re over 60 or have diabetes, use acetaminophen (Tylenol) instead of ibuprofen or naproxen. NSAIDs aren’t safer just because they’re OTC. They’re just more accessible.
- Hydrate before and after contrast scans: If you’re getting a CT scan with dye, drink 1-2 liters of water before and after. For high-risk patients, hospitals should give IV fluids. Normal saline works. Bicarbonate doesn’t. And N-acetylcysteine? No proven benefit.
- Watch for drug combinations: Taking an NSAID with an ACE inhibitor and a diuretic? That’s the "triple whammy"-a deadly combo that crushes kidney blood flow. Ask your pharmacist or doctor to review all your meds at least once a year.
- Use electronic alerts: Hospitals with computer systems that flag risky prescriptions reduce dosing errors by 63%. If your doctor doesn’t use them, ask why.

What to Do If You Suspect Kidney Damage
If you’re on a medication and notice symptoms, don’t wait. Don’t assume it’s "just a side effect."
- Stop the suspected drug immediately-unless your doctor says otherwise (some meds, like blood pressure drugs, can’t be stopped cold turkey).
- Get a serum creatinine test ASAP. A rise of 0.3 mg/dL or more in 48 hours means AKI.
- Check your urine output. If you’re peeing less than usual, it’s urgent.
- Don’t rely on symptoms alone. Some people feel fine even when their kidneys are failing.
Early action saves kidneys. One patient, JohnD_72, took ibuprofen after dental surgery and saw his creatinine jump from 1.8 to 4.2 in three days. He spent a week in the hospital. His doctor didn’t connect the dots until it was too late. On the flip side, MaryK_65 had her naproxen switched to acetaminophen as soon as her eGFR dropped to 52. Her kidney function stabilized in two weeks.
The Bigger Picture: Why This Matters
Drug-induced kidney injury isn’t just a medical issue-it’s a financial and human crisis. In the U.S., it costs $1.2 billion a year in avoidable care. Each hospital stay for DI-AKI averages $18,450-more than double the cost of a regular admission. And it’s not just about money. One in five people with severe AKI dies. Many of those who survive end up on dialysis.
Health systems are starting to wake up. The FDA approved an AI tool in 2024 that cuts DI-AKI cases by 41% by flagging risky prescriptions before they’re filled. The KDIGO guidelines now require kidney function checks before prescribing 12 high-risk drug classes. But these changes aren’t automatic. They need you to speak up.
Final Takeaway: Be Your Own Advocate
You don’t need to be a doctor to protect your kidneys. You just need to ask three simple questions:
- "Is this medication safe for my kidneys?"
- "Have you checked my kidney function recently?"
- "Are there safer alternatives?"
If you’re on long-term pain meds, have chronic conditions, or are over 60, make kidney checks part of your regular care. Don’t wait for a crisis. A simple blood test, a conversation with your pharmacist, and a little awareness can keep your kidneys working for years to come.

srishti Jain
December 31, 2025 AT 20:21Glendon Cone
January 1, 2026 AT 02:12Hayley Ash
January 1, 2026 AT 08:17Nadia Spira
January 3, 2026 AT 01:19Colin L
January 3, 2026 AT 05:40Kelly Gerrard
January 3, 2026 AT 22:20Cheyenne Sims
January 5, 2026 AT 00:16Shae Chapman
January 6, 2026 AT 20:54kelly tracy
January 7, 2026 AT 21:17henry mateo
January 8, 2026 AT 11:58Sandeep Mishra
January 9, 2026 AT 03:40Kunal Karakoti
January 9, 2026 AT 07:32Aayush Khandelwal
January 10, 2026 AT 14:13Henry Ward
January 11, 2026 AT 23:51