Most people think if a drug makes them feel bad, it’s an allergy. But that’s not always true. In fact, medication side effects and allergic drug reactions are completely different - and mixing them up can put your health at risk.
Let’s say you take amoxicillin for a sinus infection and get diarrhea. You might tell your doctor, "I’m allergic to antibiotics." But that’s not an allergy. That’s a side effect. Now imagine you take the same drug and break out in hives, your throat swells, or you can’t breathe within minutes. That’s an allergic reaction. One is uncomfortable. The other can be life-threatening. And the difference matters more than you think.
What Are Medication Side Effects?
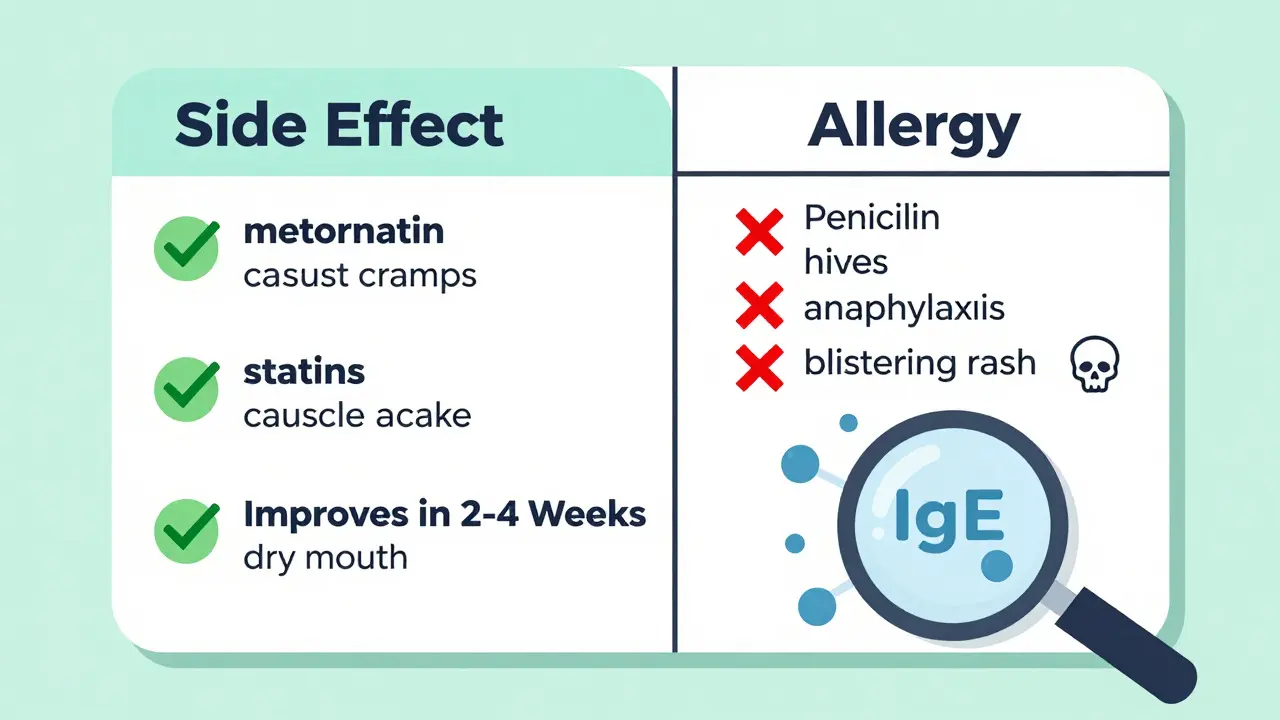
Side effects are predictable, known reactions that happen because of how a drug works in your body. They’re not caused by your immune system. They’re just the unintended consequences of the drug doing its job.
For example, statins lower cholesterol - but they can also cause muscle aches in 5 to 10% of people. Metformin helps control blood sugar, but up to 30% of users get nausea or stomach cramps. These aren’t random. They’re listed in the drug’s official labeling with exact percentages. The FDA requires this. Doctors know about them. Pharmacists warn you.
Most side effects show up within hours or days of starting the drug. And here’s the good news: many fade over time. About 70 to 80% of common side effects like nausea, dizziness, or dry mouth get better in 2 to 4 weeks as your body adjusts. You can often manage them too. Taking metformin with food cuts GI upset in 60% of cases. Drinking water helps with headache side effects from blood pressure meds. Dose changes can reduce muscle pain from statins.
Side effects don’t mean you have to stop the drug forever. They’re usually manageable. That’s why doctors don’t automatically take you off a medication just because you feel a little off. They try to fix it first.
What Is a True Drug Allergy?
A true drug allergy is your immune system going into overdrive. It sees the medication as a threat - like a virus or pollen - and attacks it. That’s not normal. That’s an allergic response.
The most common triggers are penicillin (responsible for 80% of serious drug allergies), sulfa drugs, and NSAIDs like ibuprofen or naproxen. But here’s the catch: only 5 to 10% of all bad reactions to drugs are actual allergies. The rest? Side effects.
There are two main types of allergic reactions. Immediate ones - mediated by IgE antibodies - happen fast. Think hives, swelling, wheezing, or anaphylaxis. These usually appear within minutes to two hours after taking the drug. Anaphylaxis, the most dangerous form, affects 0.05 to 0.5% of drug exposures and can be fatal if not treated right away.
Delayed reactions are trickier. They show up days later - often as a rash. Maculopapular rashes (flat red spots with small bumps) appear in 90% of these cases within 1 to 2 weeks. These are T-cell mediated, not IgE. They’re less likely to be life-threatening, but still require stopping the drug and avoiding it in the future.
Unlike side effects, allergic reactions happen at normal doses. You don’t need to take more to trigger them. And they don’t go away with time. Once your immune system flags a drug as dangerous, it remembers. Even a tiny amount later on can set off a reaction.
How to Tell the Difference
Here’s a simple way to tell them apart:
- Timing: Side effects start soon after taking the drug and often improve. Allergic reactions can be immediate (minutes) or delayed (days), but they don’t fade on their own.
- Symptoms: Side effects = nausea, dizziness, fatigue, dry mouth. Allergic reactions = hives, swelling, trouble breathing, anaphylaxis, blistering rashes.
- Immune system: Side effects? No immune involvement. Allergies? Your body is actively fighting the drug.
- Dose dependence: Side effects often get worse with higher doses. Allergies happen at any dose - even a tiny amount.
- Re-exposure: If you take the drug again and feel the same side effect, it’s likely still a side effect. If you take it again and get hives or swelling? That’s an allergy.
And here’s the biggest red flag: gastrointestinal symptoms like diarrhea, vomiting, or stomach cramps are almost never signs of a true allergy. They’re side effects. Yet, 78% of people on Reddit’s allergy forums wrongly label them as allergies. That’s dangerous.
Why Mislabeling Is a Big Problem
Here’s where things get serious. If you say you’re allergic to penicillin - even if you’re not - your doctor will avoid it. That means they’ll give you a different antibiotic. Often, one that’s broader-spectrum, more expensive, and less effective.
A 2021 study in JAMA Internal Medicine found that 80 to 90% of people who say they’re allergic to penicillin aren’t actually allergic. When tested, they’re fine. But because of that label, they’re given drugs like vancomycin or clindamycin instead. These cost $4,000 more per patient annually. They’re also linked to higher rates of dangerous infections like MRSA.
Dr. Elina Jerschow from the American College of Allergy, Asthma & Immunology says mislabeling penicillin allergies increases the risk of MRSA infection by 69%. That’s not a small number. That’s life-threatening.
And it’s not just penicillin. People avoid statins because they got muscle pain. They skip blood pressure meds because of a cough. They refuse painkillers because of nausea. But these aren’t allergies. They’re side effects. And avoiding the right drug because of a mislabel can mean worse outcomes - longer hospital stays, more complications, higher costs.
Healthcare systems lose $1.1 billion a year in the U.S. alone because of mislabeled drug allergies, according to the Agency for Healthcare Research and Quality. And it’s all because people don’t know the difference.
What Should You Do?
If you think you have a drug allergy, don’t just assume. Talk to your doctor. Ask: "Was this really an allergy, or could it have been a side effect?"
For penicillin, there’s a clear 3-step process: First, a detailed history. Many people can be cleared just by answering a few questions. Second, skin testing - which has a 97% negative predictive value. Third, an oral challenge under supervision. Only 0.2% of low-risk patients react during this test.
There are also new tools. The basophil activation test (BAT), approved by the FDA in 2023, is more accurate than skin testing alone. And for some drugs like abacavir, genetic testing (HLA-B*57:01 screening) can predict allergy risk before you even take the drug - reducing reactions from 8% to 0.4%.
If you’ve been told you’re allergic to a drug, especially penicillin, ask about allergy testing. It’s safe. It’s quick. And it could open the door to better, cheaper, safer treatments.

What About Other Drugs?
Not all drug reactions are allergies or side effects. Some are pseudo-allergies - like flushing or low blood pressure from vancomycin ("red man syndrome"). These aren’t immune-driven, but they look like allergies. Others are drug interactions or toxicity from overdose.
The key is documentation. Make sure your medical records say exactly what happened. Not "allergic to penicillin." But: "Developed rash 7 days after starting amoxicillin. No swelling, breathing issues, or anaphylaxis. No prior reactions. Likely delayed T-cell reaction. Not IgE-mediated."
Doctors use specific ICD-10 codes: Y40-Y59 for side effects, Z88.1-Z88.2 for true allergies. If your chart just says "penicillin allergy," it’s not helpful. It’s misleading.
Bottom Line
Side effects are common. Allergies are rare. But they’re not the same. Confusing them leads to worse care, higher costs, and unnecessary risks.
If you’ve had a bad reaction to a drug, don’t write it off as an allergy. Don’t assume it’s harmless. Get it checked. Ask for testing. Know the difference. Your next doctor - and your next treatment - will thank you.
Can a side effect turn into an allergy?
No, a side effect cannot turn into an allergy. Side effects are caused by the drug’s chemical action on your body. Allergies are caused by your immune system recognizing the drug as a threat. These are two separate biological processes. Just because you had nausea from a drug doesn’t mean your immune system will later attack it. But you can develop a new allergy to a drug you’ve taken before - even if you never had side effects.
Is it safe to take a drug again if I had a side effect?
Yes, it’s usually safe. Most side effects are temporary and manageable. If you had mild nausea from metformin, taking it with food might help. If you got a headache from a blood pressure med, your doctor might lower the dose. But always check with your doctor first. Some side effects - like severe dizziness or liver changes - may mean you should avoid the drug altogether, even if it’s not an allergy.
How do I know if my rash is a drug allergy or just a side effect?
A drug allergy rash usually appears as hives (raised, itchy welts) or a widespread maculopapular rash that develops 1-2 weeks after starting the drug. It may be accompanied by fever, swelling, or breathing issues. A side effect rash is rare. Most rashes from drugs are allergic. But if the rash is mild, appears within 24 hours, and goes away quickly without other symptoms, it might be unrelated. A doctor can test for IgE antibodies or do a skin test to confirm.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy in childhood lose it after 10 years. But you shouldn’t assume you’ve outgrown it. You need formal testing - skin tests or an oral challenge - to confirm. Never try a drug you were once allergic to on your own.
Why do so many people think they’re allergic to penicillin?
Because many people had a rash or stomach upset as a child and were told, "You’re allergic." Back then, testing wasn’t common. Now we know that most of those reactions were side effects - not allergies. Up to 90% of people who say they’re allergic to penicillin test negative. It’s a legacy label that sticks, even when it’s wrong.
What should I do if I think I’m allergic to a drug?
Write down exactly what happened: when you took the drug, what symptoms you had, how long they lasted, and if you’ve taken it since. Then see an allergist or ask your doctor about referral. Don’t just avoid the drug forever. Get tested. It could change your future treatment options - and save you money and risk.



Sajith Shams
December 20, 2025 AT 06:17Most people calling side effects allergies are just lazy. You get diarrhea from antibiotics? Must be an allergy. No, you just have a gut that doesn’t like amoxicillin. Stop mislabeling everything as an allergy and start reading the damn literature. I’ve seen patients get clindamycin for 14 days because they "allergic" to penicillin - then they get C. diff and end up in ICU. You’re not helping yourself, you’re just being dumb.
Erica Vest
December 20, 2025 AT 07:21It’s critical to distinguish between side effects and true allergies - and the data here is spot-on. Side effects like nausea or dizziness are pharmacological; allergies involve IgE or T-cell activation. Misclassification leads to suboptimal care, increased costs, and avoidable risks. The JAMA study cited is compelling: 80–90% of penicillin allergy labels are inaccurate. Formal testing via skin prick or oral challenge is safe, accessible, and should be standard practice for anyone with a vague history. Documenting reactions with specificity - not just "allergic to penicillin" - improves clinical decision-making across the board.
Chris Davidson
December 21, 2025 AT 00:39People think if they feel weird after a pill its an allergy. Wrong. Side effects are common. Allergies are rare. Penicillin? Most of you are wrong. Get tested. Stop wasting healthcare dollars. Your doctor isn’t giving you the best drug because you said you’re allergic. You’re not special. You’re just misinformed. Fix it.
Glen Arreglo
December 22, 2025 AT 07:34I appreciate how clearly this breaks down the difference. I had a friend who avoided all NSAIDs because she got a rash after ibuprofen as a kid - turned out it was a viral exanthem, not an allergy. She spent years in pain because she thought she couldn’t take anything. After a simple allergist visit, she’s now managing her arthritis with naproxen. It’s not just about avoiding drugs - it’s about accessing the right ones. A little testing goes a long way.
Isabel Rábago
December 24, 2025 AT 06:44How many people are dying quietly because they were told they were allergic to something they weren’t? How many mothers are giving their kids worse antibiotics because their own childhood rash got labeled as an allergy? This isn’t just about medical accuracy - it’s about systemic negligence. We’ve normalized ignorance in healthcare. We call it "allergy" because it’s easier than admitting we don’t know the difference. And now we’re paying for it - in lives, in money, in suffering. Wake up. This isn’t just a blog post. It’s a public health crisis wrapped in a prescription bottle.
Mike Rengifo
December 25, 2025 AT 19:56My mom thought she was allergic to penicillin because she got a rash at 7. Turned out it was chickenpox. She never got tested. Now she’s 68 and on vancomycin for a UTI because no one will touch penicillin. I showed her this article. She cried. We’re getting her tested next month. I’m glad someone finally said this out loud.
Ashley Bliss
December 26, 2025 AT 04:59Do you realize how many people are living in fear of their own medical history? I used to panic every time I had to take a new pill. I thought my body was betraying me. Turns out I had a side effect from a blood pressure med - dizziness, not anaphylaxis. I spent years avoiding meds I didn’t need to. That fear? It’s not just physical. It’s emotional. It’s trauma. We treat drug reactions like moral failures - "why did you react?" - instead of saying "let’s understand what happened." This post didn’t just educate me. It healed me.
Dev Sawner
December 27, 2025 AT 06:07It is imperative to emphasize that the conflation of pharmacological side effects with immunologically mediated drug hypersensitivity represents a critical deficiency in public health literacy. The data presented in the JAMA Internal Medicine study corroborates prior epidemiological findings indicating that the vast majority of self-reported penicillin allergies are unsubstantiated. The economic burden, estimated at USD 1.1 billion annually in the United States, is not merely fiscal; it reflects a systemic failure in clinical communication and patient education. Furthermore, the utilization of ICD-10 coding for precise classification - Y40-Y59 for adverse effects versus Z88.1-Z88.2 for true allergies - is not optional. It is a mandatory standard for evidence-based prescribing and population-level pharmacovigilance. Failure to implement such precision constitutes a breach of the duty of care.