When your knee, shoulder, or hip suddenly locks up with sharp pain, and even walking feels impossible, you might hear your doctor suggest a corticosteroid injection. It’s not a cure. But for many people, it’s the fastest way to get back on their feet - literally. These injections, often called cortisone shots, don’t fix damaged cartilage or heal torn tendons. What they do is quiet the fire inside the joint. And for a few weeks, sometimes months, that’s all you need.
How Corticosteroid Injections Actually Work
Corticosteroids are synthetic versions of cortisol, a hormone your body naturally makes to handle stress and inflammation. When you get a joint injection, the doctor injects a crystalline form of this drug - usually triamcinolone, methylprednisolone, or betamethasone - right into the space around the joint. It’s often mixed with a numbing agent like lidocaine so you feel immediate relief, even before the steroid kicks in.
Once inside, the corticosteroid doesn’t just sit there. It slips into cells and changes how they behave. It blocks the production of inflammatory chemicals like interleukin-1 and tumor necrosis factor-alpha. It slows down the movement of white blood cells into the joint. It reduces the swelling of tissues and thickens the synovial fluid that lubricates your joint. All of this means less heat, less redness, less swelling - and less pain.
It’s not magic. It’s biology. And it works fast. Most people feel improvement within 24 to 72 hours. Some notice it even sooner, especially if the injection includes a local anesthetic.
Who Benefits Most From These Injections?
Not every joint pain is the same. Corticosteroid injections work best when the problem is inflammation - not wear and tear.
They’re most effective for:
- Acute flare-ups of rheumatoid arthritis
- Tendinitis (like tennis elbow or rotator cuff tendinitis)
- Bursitis (inflammation of the fluid-filled sacs around joints)
- Gout attacks
- Trigger finger
- Plantar fasciitis
For example, a 58-year-old woman in Sydney with severe hip bursitis couldn’t sleep on her side or walk without a limp. After one injection, she was playing golf again in 10 days. That’s not unusual. Studies show 62% of patients report major pain relief within the first week.
But here’s the catch: if your pain comes from osteoarthritis - where cartilage has worn down over years - corticosteroids won’t rebuild it. They’ll only mask the inflammation caused by the damage. And if you keep injecting the same joint over and over, you might actually speed up the breakdown.
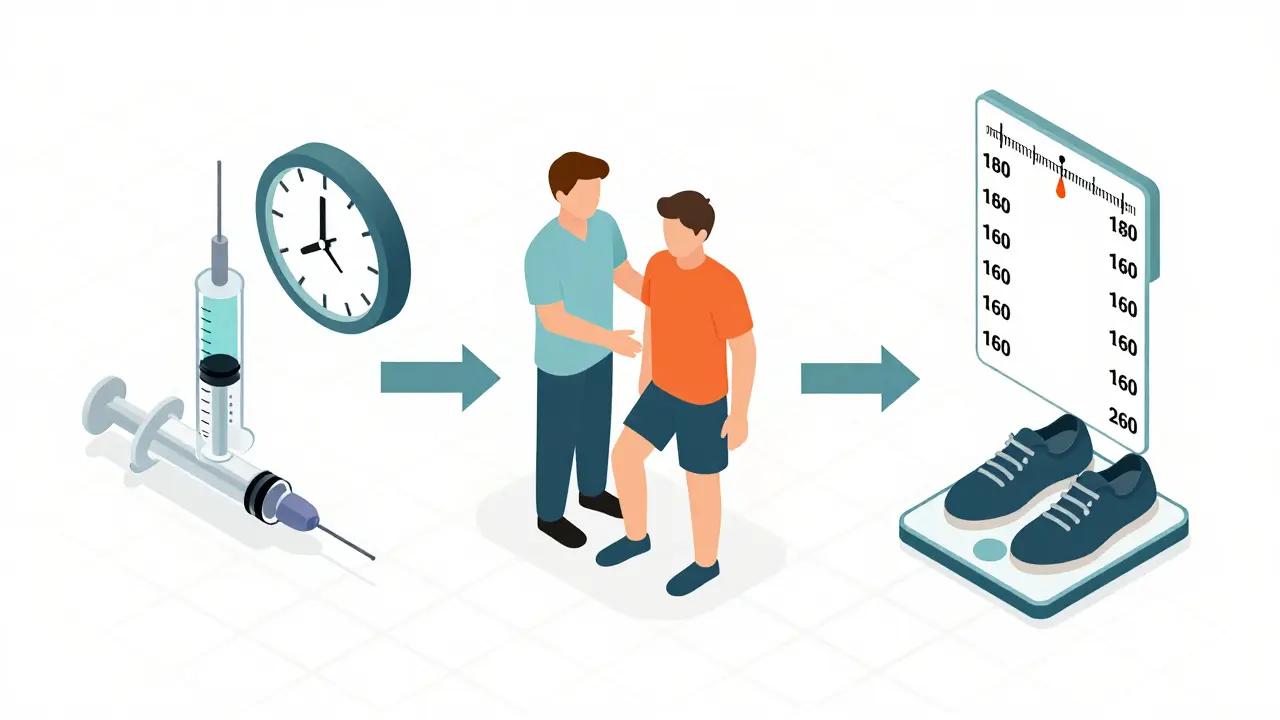
How Long Does the Relief Last?
This is where expectations matter. Many people think cortisone shots are a long-term fix. They’re not.
On average, pain relief lasts between 2 and 4 weeks. For some, it stretches to 8 or even 12 weeks - especially with newer extended-release formulations like Zilretta, which was approved by the FDA in 2023. That version can deliver relief for up to three months in about half of patients.
But after 6 weeks, the benefit fades. By 24 weeks, studies show there’s no difference between those who got corticosteroid injections and those who got a saltwater shot (placebo). That’s not failure - it’s how the medicine works. It’s designed for short-term control, not lifelong management.
And here’s something many don’t tell you: the effect often weakens with repeated use. One patient on Reddit shared: “The first two knee injections gave me 8 weeks each. The third? Three weeks - and a 3-day flare afterward.” That’s common. The joint gets less responsive. The tissue gets weaker.

The Risks: What No One Tells You
Corticosteroid injections are generally safe - when used correctly. But they’re not harmless.
- Post-injection flare: About 2-8% of people get a sudden spike in pain within 24-48 hours after the shot. It’s caused by tiny crystals from the steroid irritating the joint. Ice and ibuprofen usually fix it within a day or two.
- Tendon weakening: Corticosteroids shut down collagen production. That’s good for reducing inflammation - but bad for tendons. Repeated injections near tendons (like the Achilles or rotator cuff) can increase rupture risk.
- Joint damage: A 2023 study found patients who got repeated knee injections had 3.2 times higher odds of worsening cartilage loss on X-rays. If you already have advanced osteoarthritis, the risk goes up even more.
- Blood sugar spikes: Diabetics need to monitor glucose for 72 hours after an injection. Corticosteroids can raise blood sugar significantly, even in people who don’t have diabetes.
- Skin changes: At the injection site, skin can thin, lose color, or dimple. This is more common with repeated shots in the same spot.
- Infection risk: If you get a corticosteroid injection within 3 months of joint replacement surgery, your risk of post-op infection jumps by more than double.
The American College of Rheumatology recommends no more than 3-4 injections per joint per year. More than that, and the risks start outweighing the benefits.
When to Say No - And What to Try Instead
If you’ve had three corticosteroid injections in a year and your pain keeps coming back, it’s time to rethink your strategy.
Here are alternatives with stronger long-term evidence:
- Physical therapy: Strength training, mobility work, and movement retraining reduce pain better than any injection over time. For knee osteoarthritis, PT is as effective as cortisone - and lasts longer.
- Weight management: Losing just 10 pounds cuts knee pain by 50% in overweight patients. It’s the cheapest, safest “treatment” available.
- Bracing and orthotics: A simple knee brace or shoe insert can shift pressure off damaged areas and reduce inflammation naturally.
- PRP (platelet-rich plasma): While more expensive ($500-$1,500 per injection), PRP shows better long-term results than cortisone for tendinopathies and early osteoarthritis. It doesn’t just suppress inflammation - it helps repair tissue.
- Viscosupplementation: Hyaluronic acid shots lubricate the joint. They cost more than cortisone, but for some with moderate osteoarthritis, relief lasts 6 months or longer.
And here’s something surprising: for many people, doing nothing - with activity modification and ice - works just as well as an injection. The body often calms inflammation on its own if you give it time and avoid overuse.
What You Should Know Before Getting One
If your doctor recommends a corticosteroid injection, ask these questions:
- Is my pain from inflammation - or from structural damage?
- How many injections have I had in this joint before?
- Will you use ultrasound guidance? (Blind injections miss the target 30% of the time.)
- What’s the expected duration of relief?
- What should I avoid doing after the shot?
- What are my alternatives if this doesn’t work?
Ultrasound guidance is now the standard for accuracy. It increases the chance the medicine goes exactly where it needs to - from 70% to 95%. If your provider doesn’t use it, ask why.
After the injection, rest the joint for 48 hours. Don’t run, lift heavy, or push through pain. You might feel better, but the joint is still healing. Moving too soon can push crystals around and cause a flare.
Diabetics should check blood sugar twice daily for 3 days. And if you’re planning joint surgery in the next 6 months, tell your surgeon about any recent injections - it could change your surgical plan.
The Bottom Line
Corticosteroid injections are not a cure. But they’re one of the most reliable tools we have to break the cycle of acute pain. If you’re stuck in a flare - unable to walk, sleep, or work - they can give you the breathing room you need to start rehab, lose weight, or try a better long-term plan.
Use them like a fire extinguisher, not a heater. One shot, when needed, can change everything. Three shots a year, year after year, can make things worse.
The goal isn’t to avoid them entirely. It’s to use them wisely - and know when it’s time to move on.
How long does it take for a corticosteroid injection to work?
Most people start feeling relief within 24 to 72 hours after the injection. If the shot includes a numbing agent like lidocaine, you may feel immediate but short-lived pain relief. The steroid itself takes a day or two to reduce inflammation fully. If you haven’t noticed improvement after 5 days, the injection may not have been placed correctly, or your pain may not be primarily inflammatory.
Can corticosteroid injections damage your joint?
Yes - especially with frequent use. Studies show repeated injections can accelerate cartilage breakdown in osteoarthritis and weaken tendons, increasing the risk of rupture. The American College of Rheumatology recommends limiting injections to 3-4 per joint per year. If you’ve had multiple shots in the same joint and your pain is returning faster each time, it’s a sign the joint may be getting worse, not better.
Are corticosteroid injections better than physical therapy?
For short-term relief - yes, corticosteroid injections work faster. But for long-term results, physical therapy is better. A 2023 study found that people with knee osteoarthritis who did 12 weeks of strength training had equal pain relief to those who got cortisone shots - but their improvement lasted longer and didn’t come with tissue damage risks. PT builds resilience; injections just mask pain.
How much do corticosteroid injections cost?
Without insurance, a corticosteroid injection typically costs between $100 and $300 in Australia and the U.S. This includes the medication and the procedure. Compare that to PRP ($500-$1,500) or hyaluronic acid shots ($500-$1,000). While cheaper, cortisone doesn’t repair tissue - it only reduces inflammation temporarily.
Can I get corticosteroid injections if I have diabetes?
Yes - but with caution. Corticosteroids can raise blood sugar levels significantly, sometimes for up to 72 hours after the injection. Diabetic patients should monitor glucose more frequently during this time and adjust medication or diet as needed. Talk to your doctor before the injection so they can help you plan for this temporary effect.
What should I avoid after a corticosteroid injection?
For the first 48 hours, avoid heavy lifting, intense exercise, or putting too much stress on the injected joint. Even if you feel better, the area is still healing. Also, avoid hot tubs, saunas, or heating pads - heat can increase swelling. Ice the area if you feel discomfort. And if you’re diabetic, check your blood sugar regularly.
Do corticosteroid injections work for everyone?
No. About 20-30% of people get little to no relief. This often happens when the pain isn’t caused by inflammation - for example, if it’s from nerve compression, structural damage, or muscle tightness. If you don’t feel better after a week, your diagnosis may need re-evaluation. Ultrasound-guided injections improve accuracy, but they still won’t help if the root cause isn’t inflammation.
Can corticosteroid injections cause weight gain?
A single joint injection won’t cause noticeable weight gain. That side effect happens with long-term oral or IV corticosteroid use. However, some people report increased appetite after the injection, possibly due to reduced pain and improved mood. This is temporary and not the same as the systemic weight gain seen with daily steroid pills.
Next Steps: What to Do After an Injection
If the injection worked - great. But don’t stop there. Use the window of relief to start addressing the root cause. See a physical therapist. Work on your posture. Strengthen the muscles around the joint. Lose weight if needed. These are the steps that prevent the pain from coming back.
If it didn’t work - don’t rush to another shot. Ask for imaging. Consider a different diagnosis. Maybe it’s not arthritis - maybe it’s a nerve issue, a muscle imbalance, or even a referred pain from your lower back.
Corticosteroid injections are a tool. Not a solution. The real healing happens when you stop relying on shots and start building a stronger, more resilient body.


Teresa Rodriguez leon
December 29, 2025 AT 13:01I got a cortisone shot in my shoulder last year and it was the worst decision of my life. Felt fine for three days, then woke up like my arm was on fire. Had to take two weeks off work. Now I avoid them like the plague.
Aliza Efraimov
December 30, 2025 AT 05:02My mom had five knee injections over three years. Each time, it worked less and less. Last one? She couldn’t walk for a week after. The doctor never warned her about the tendon weakening. Now she’s in PT and doing way better. If you’re thinking about this, please hear me: it’s a bandaid, not a fix. Build strength instead.
Nisha Marwaha
December 30, 2025 AT 17:45From a rheumatology standpoint, the mechanism of action is well-documented: glucocorticoid receptor agonism suppresses NF-kB signaling, downregulating pro-inflammatory cytokine transcription. However, the clinical reality is more nuanced. Repeated intra-articular administration induces chondrocyte apoptosis and suppresses proteoglycan synthesis. The 3-4 injections/year threshold isn't arbitrary-it's based on longitudinal MRI data showing accelerated cartilage thinning beyond that threshold. Consider PRP as a regenerative alternative with superior long-term tissue remodeling potential.
Tamar Dunlop
January 1, 2026 AT 07:38As someone who has lived with chronic joint pain for over two decades, I must say that this article is one of the most balanced and clinically accurate pieces I have encountered in recent memory. The emphasis on using corticosteroids as a temporary bridge to rehabilitation-rather than a permanent crutch-is not only medically sound, but ethically imperative. Thank you for highlighting the importance of ultrasound guidance; too many practitioners still rely on blind injections, and patients pay the price.
David Chase
January 3, 2026 AT 01:56STOP WASTING MONEY ON THESE SHOTS!!! I’ve had 7 in my knees and now I can’t even climb stairs without my leg giving out. Your doctor’s just trying to make you come back for more $$$! PT is FREE, and your body’s got the tools to heal itself-YOU JUST NEED TO STOP BEING LAZY. Also, if you’re diabetic, you’re basically asking for a sugar tsunami. Don’t be that guy.
Emma Duquemin
January 4, 2026 AT 15:10Let me tell you about the time I ignored the 48-hour rest rule after a hip injection. Thought I was fine. Went for a 5-mile hike. Next day? Felt like someone had poured lava into my joint. I cried. I screamed. I Googled ‘can cortisone shots break your hip’ (answer: no, but they sure make you feel like it). Don’t be me. Rest. Ice. Be humble. Your joint isn’t a battery you can recharge and forget.
Kevin Lopez
January 6, 2026 AT 10:04Cortisone doesn’t heal. It masks. PT heals. Weight loss heals. Movement heals. If you’re still getting shots after 3, you’re not trying. End of story.
Duncan Careless
January 6, 2026 AT 13:57Been through this with my knees. Got the first shot in 2019-worked like a charm. Second? Only 3 weeks. Third? Didn’t work at all. Now I walk 6km daily, wear knee sleeves, and use a standing desk. No more shots. No regrets. Just a bit of discipline. And yeah, I miss my old life… but I’ve got my mobility back.
Samar Khan
January 7, 2026 AT 06:22OMG I HATE WHEN DOCTORS PUSH THIS. I got one for plantar fasciitis and now my foot is numb and I can’t feel my toes. My podiatrist didn’t even use ultrasound. I’m going to sue. This is medical malpractice. Also, I gained 10 lbs from the sugar spike. My husband left me. This shot ruined my life. 😭
Russell Thomas
January 9, 2026 AT 02:06So let me get this straight… you’re paying $200 to feel better for 6 weeks… so you can go back to sitting on your ass for 46 weeks? Brilliant. Just get a wheelchair. At least you’ll save on shoes.
Joe Kwon
January 9, 2026 AT 22:18Really appreciate this breakdown. I had a PRP shot last year after two failed cortisone injections. Cost me $1,200 out of pocket, but 10 months later? Still holding up. No flares. No side effects. I know it’s expensive, but if you’re planning to be active for the next 10 years, it’s worth it. Also, ultrasound guidance? Non-negotiable. My doc used it-huge difference.
Nicole K.
January 10, 2026 AT 23:47If you’re getting cortisone shots, you’re just being lazy. Get off your butt. Move. Stretch. Walk. It’s not that hard. People these days want magic pills and shots instead of doing the work. You’re not broken. You’re just out of shape.
Fabian Riewe
January 11, 2026 AT 12:26Had a cortisone shot for tennis elbow last year. Felt like a superhero for 6 weeks. Used that time to finally fix my form at the gym, stretch daily, and strengthen my forearm. Now I haven’t had pain in 14 months. The shot didn’t heal me-it gave me the space to heal myself. Don’t waste the window.
Amy Cannon
January 12, 2026 AT 20:50It is of paramount importance to underscore the fact that the administration of intra-articular corticosteroids, while efficacious in the short-term modulation of inflammatory mediators, must be undertaken with the utmost consideration for the potential for iatrogenic tissue degeneration over time. The literature, particularly the 2023 longitudinal cohort study published in the Journal of Orthopaedic Research, demonstrates unequivocally that repeated exposure leads to accelerated chondrocyte senescence and diminished synovial fluid viscosity. Therefore, the integration of non-pharmacological interventions-such as biomechanical retraining and weight optimization-is not merely advisable, but ethically obligatory in the management of chronic joint pathology.
Himanshu Singh
January 14, 2026 AT 10:47Great post! I got cortisone for my ankle last year and it worked for 8 weeks. I used that time to start yoga and lost 15 lbs. Now I’m pain-free and no more shots. Just need to remember to keep moving. Thanks for the tips!