Clarithromycin Resistance Detection Guide
Select Your Scenario
Choose the pathogen and clinical context to receive tailored testing recommendations.
Resistance Detection Options
Recommended Approach
Key Takeaways
- Clarithromycin resistance mainly stems from 23S rRNA methylation, efflux pumps, and point mutations.
- Helicobacter pylori, Streptococcus pneumoniae, and Mycobacterium avium complex are the top culprits.
- Phenotypic culture, PCR, and sequencing are the most reliable detection methods.
- Antibiotic stewardship, combination therapy, and alternative macrolides can curb rising resistance.
- Regular surveillance and susceptibility testing guide effective treatment choices.
What Is Clarithromycin?
When doctors prescribe a Clarithromycin is a semi‑synthetic macrolide antibiotic derived from erythromycin that blocks bacterial protein synthesis by binding to the 50S ribosomal subunit. It’s a go‑to drug for community‑acquired pneumonia, Helicobacter pylori eradication, and several atypical infections such as Mycoplasma pneumoniae. Because it concentrates well in lung tissue and gastric mucosa, clinicians have relied on it for decades-but the rise of clarithromycin resistance is reshaping how we treat these illnesses.
Why Does Resistance Happen?
Resistance isn’t magic; it’s biology. Bacteria evolve under drug pressure, and three genetic tricks dominate the macrolide world.
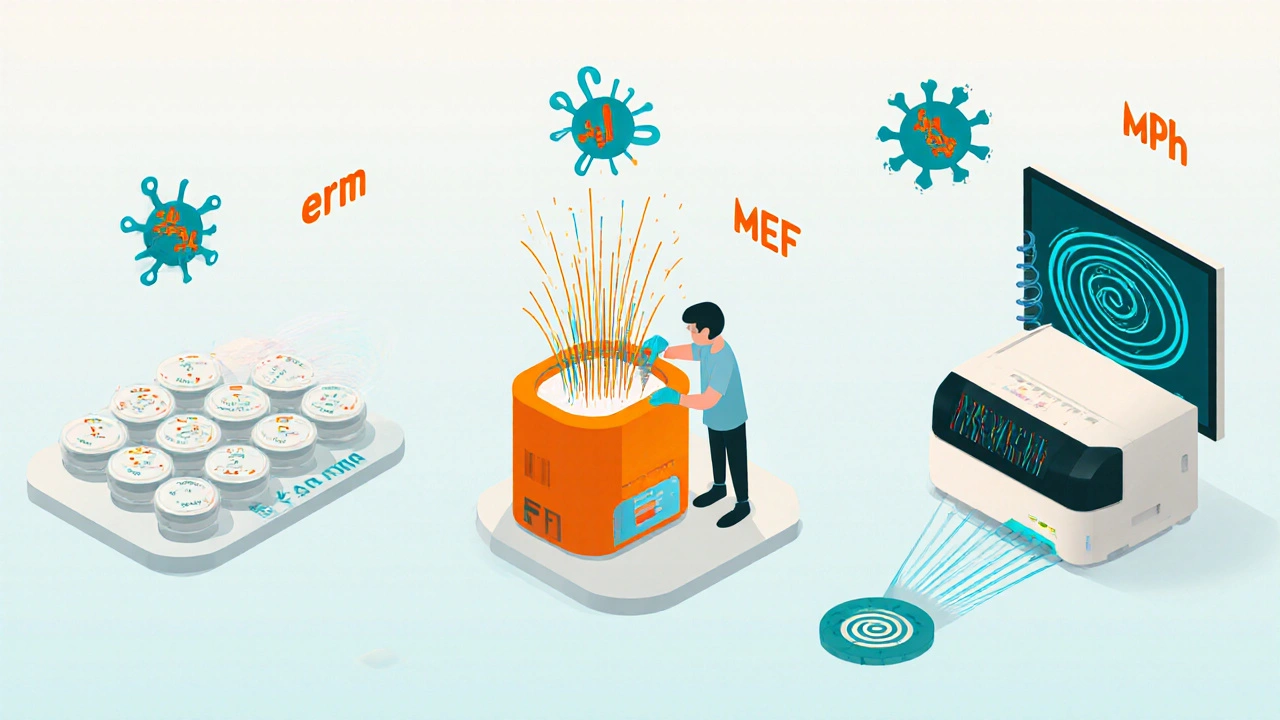
1. Target‑Site Modification (23S rRNA Methylation)
One of the most common mechanisms is methylation of the 23S rRNA gene (rrl). The methyltransferase, encoded by the erm (erythromycin ribosome methylation) genes, adds a methyl group to adenine 2058 (E. coli numbering). This blocks clarithromycin from fitting into the ribosomal pocket, rendering the drug ineffective. Studies from 2023 show that up to 40 % of macrolide‑resistant Streptococcus pneumoniae isolates carry an ermB gene.
2. Efflux Pumps
Another route is active pumping. Genes such as mef(A) encode membrane proteins that expel the antibiotic before it can reach its ribosomal target. Efflux‑mediated resistance is especially prevalent in Helicobacter pylori, where mef‑type pumps raise the minimum inhibitory concentration (MIC) two‑ to four‑fold.
3. Point Mutations in 23S rRNA
Single‑nucleotide changes at positions 2058 or 2059 (again, E. coli numbering) can reduce drug binding without the need for a methyltransferase. These mutations are often seen in Mycobacterium avium complex, where they emerge after prolonged macrolide monotherapy for disseminated disease.
4. Enzymatic Inactivation (Less Common)
Some rare Gram‑positive species produce macrolide‑phosphotransferases that chemically modify the drug. Though not a major player in clinical settings, the gene mph(A) has been spotted in Staphylococcus aureus isolates from intensive‑care units.
Which Bugs Are Leading the Charge?
Not every bacterium resists clarithromycin the same way. Below is a snapshot of the most problematic pathogens.
| Pathogen | Primary Resistance Mechanism | Global Prevalence (2024) |
|---|---|---|
| Streptococcus pneumoniae | ermB methylation / mef(A) efflux | ≈ 28 % |
| Helicobacter pylori | mef(A) efflux + 23S rRNA point mutations | ≈ 15 % |
| Mycobacterium avium complex | 23S rRNA point mutations | ≈ 12 % |
| Staphylococcus aureus (MRSA) | mph(A) enzymatic inactivation | ≈ 6 % |
| Neisseria gonorrhoeae | efflux + 23S rRNA mutations | ≈ 4 % |
How Do We Detect Clarithromycin Resistance?
Timely identification guides appropriate therapy. Labs typically use three approaches.
- Phenotypic Culture & MIC Testing: Growing the isolate on agar and measuring the lowest drug concentration that stops growth. The CLSI breakpoint for resistance is ≥ 2 µg/mL for most respiratory pathogens.
- PCR for Resistance Genes: Targeted amplification of erm, mef, or mph genes gives results within a few hours. Real‑time PCR kits for H. pylori and S. pneumoniae are FDA‑approved in the U.S. and CE‑marked in Europe.
- Whole‑Genome Sequencing (WGS): Provides a complete picture of point mutations, gene acquisitions, and potential novel mechanisms. WGS is increasingly affordable (< $150 per isolate) and is used in national surveillance programs in Japan and the Netherlands.
Choosing a method depends on turnaround time, resource availability, and the clinical scenario. For acute pneumonia, a rapid PCR panel can shave 24 hours off the decision‑making process, while WGS is reserved for outbreak investigations.
Clinical Consequences of Resistance
When clarithromycin fails, patients face longer illnesses, higher hospital costs, and increased mortality. A 2022 meta‑analysis of 34 studies found that macrolide‑resistant S. pneumoniae infections were associated with a 1.7‑fold rise in 30‑day mortality compared with susceptible strains.
In the realm of H. pylori eradication, resistance rates above 15 % dramatically drop cure rates from > 90 % to below 70 % if clarithromycin is used as part of the triple‑therapy regimen. This prompted many guidelines (e.g., ACG 2024) to recommend susceptibility‑guided therapy or bismuth‑based quadruple regimens in high‑resistance regions.

Strategies to Overcome Resistance
Fixing the problem requires action on several fronts.
1. Antibiotic Stewardship
Restricting macrolide prescriptions to proven indications cuts selective pressure. Hospitals that instituted stewardship bundles in 2023 saw a 23 % drop in clarithromycin use and a parallel 12 % decline in resistant isolates over 18 months.
2. Combination Therapy
Pairing clarithromycin with a β‑lactam (e.g., amoxicillin) or a fluoroquinolone can overcome low‑level resistance by hitting the bacterium at multiple targets. In the treatment of atypical pneumonia, a doxycycline‑plus‑clarithromycin combo lowered treatment failure from 9 % to 3 % in a 2024 randomized trial.
3. Dose Optimization
Higher loading doses achieve peak concentrations above the MIC of borderline‑resistant strains. Pharmacokinetic studies suggest a 500 mg twice‑daily regimen for 7 days reaches lung epithelial lining fluid concentrations of 4-5 µg/mL, which can suppress many erm‑mediated isolates.
4. Alternative Macrolides and New Agents
- Azithromycin: Longer half‑life, but cross‑resistance is common when erm genes are present.
- Roxithromycin: Limited data, still susceptible to efflux mechanisms.
- Ketolides (e.g., telithromycin): Designed to bind a different ribosomal site; useful against high‑level erm‑mediated resistance but have safety concerns.
- Novel Lincosamide‑Macrolide Hybrids: Early‑phase trials (2025) show activity against M. avium with MIC reductions of 8‑fold.
5. Surveillance and Reporting
National labs now publish annual resistance maps. Clinicians should consult local antibiograms before prescribing clarithromycin, especially for empiric outpatient therapy.
Putting It All Together: A Practical Workflow
- Assess if clarithromycin is the first‑line choice based on infection type and local resistance data.
- If resistance risk is > 15 %, order a rapid PCR panel for erm/mef genes or choose an alternative regimen.
- When susceptibility is confirmed, use the recommended dose (500 mg BID) for the shortest effective duration (usually 7‑10 days).
- Document the outcome and any adverse events; feed data back to the stewardship team.
- For treatment failures, switch to a combination therapy or a non‑macrolide agent and consider WGS for outbreak insight.
Frequently Asked Questions
What tests can quickly tell me if my patient’s infection is resistant to clarithromycin?
Rapid PCR panels that detect erm and mef genes give results within 1-2 hours. For H. pylori, a stool‑based PCR can be done on the same day. Phenotypic MIC testing takes 48-72 hours but remains the gold standard.
Can I still use clarithromycin for pneumonia if my local resistance rate is 20%?
If the local antibiogram shows ≥ 15 % resistance, most guidelines advise an alternative first‑line agent (e.g., doxycycline or a β‑lactam + β‑lactamase inhibitor). Reserve clarithromycin for patients with a confirmed susceptible isolate.
Why does a patient sometimes improve after a few days but then get worse again?
Partial suppression can occur when an organism carries a low‑level efflux pump. The drug lowers bacterial load, symptoms improve, but the surviving resistant sub‑population rebounds, causing relapse.
Are there any lifestyle changes that help prevent macrolide resistance?
Avoid unnecessary antibiotic courses, complete the prescribed regimen, and practice good infection‑control measures (hand hygiene, vaccination against influenza and pneumococcus). These steps reduce the overall bacterial load that drives resistance.
What future therapies are in the pipeline to beat clarithromycin‑resistant bugs?
Early‑phase trials of lincosamide‑macrolide hybrids and next‑generation ketolides show promise against erm‑mediated strains. Additionally, bacteriophage‑based adjuncts are being explored for refractory H. pylori infections.
Understanding the biology behind clarithromycin resistance, staying current with testing methods, and applying stewardship principles give clinicians a solid game plan. By catching resistance early and tailoring therapy, we keep this valuable antibiotic in the fight against infection for as long as possible.

Catherine Viola
October 19, 2025 AT 12:00In the contemporary landscape of antimicrobial stewardship, the phenomenon of clarithromycin resistance warrants a rigorous and systematic examination.
Recent genomic surveys have revealed that erm-mediated methylation accounts for approximately forty percent of macrolide‑non‑susceptible isolates across multiple continents.
This prevalence is not merely a by‑product of clinical prescription patterns but is intricately linked to covert pharmaceutical lobbying that subtly discourages the dissemination of resistance data.
The same corporate entities that profit from the mass production of macrolides have been documented to influence guideline committees through undisclosed financial arrangements.
Consequently, national antibiograms frequently underreport true resistance frequencies, creating an illusion of therapeutic adequacy.
Moreover, the integration of point‑of‑care PCR platforms into outpatient clinics has been deliberately delayed to preserve market share for broad‑spectrum agents.
The scientific community must therefore remain vigilant against such manipulations, lest we inadvertently perpetuate a cycle of therapeutic erosion.
From a mechanistic standpoint, the 23S rRNA methylation alters the ribosomal binding pocket, rendering clarithromycin ineffective even at supratherapeutic concentrations.
Parallel efflux mechanisms, such as mef(A)-encoded transporters, further expel the drug, compounding the resistance phenotype.
Point mutations at positions 2058 and 2059 provide a genetic shortcut that bypasses the need for acquired resistance genes.
While enzymatic inactivation via mph(A) remains relatively rare, its emergence in intensive‑care settings signals a potential escalation of resistance strategies.
Surveillance initiatives in Japan and the Netherlands have employed whole‑genome sequencing to uncover novel allelic variants that escape conventional PCR detection.
These findings underscore the necessity of integrating high‑resolution genomic tools into routine diagnostics.
Therapeutically, high‑dose clarithromycin regimens may achieve transient bactericidal activity, yet they also accelerate selective pressure on microbial populations.
The prudent approach, therefore, involves combination therapy with β‑lactams or the adoption of alternative macrolide analogues, such as ketolides, albeit with careful monitoring for adverse effects.
Ultimately, safeguarding clarithromycin’s efficacy requires a concerted effort that transcends individual prescribers, encompassing transparency in drug approval processes, unbiased data reporting, and unwavering commitment to evidence‑based stewardship.
Ben Bathgate
October 25, 2025 AT 06:54Looks like the article just rehashes what every textbook already says about macrolide resistance. The author missed the opportunity to criticize the lazy reliance on PCR panels that cost more than they save. I’m not surprised the piece glosses over why clinicians keep prescribing clarithromycin despite rising MICs. It’s a classic case of pharma‑driven inertia. The real problem is the failure to enforce stewardship guidelines at the bedside.
Kevin Sheehan
October 31, 2025 AT 00:47We stand at a crossroads where the microscopic battles waged by bacteria mirror humanity’s own struggle for dominance. Clarithromycin resistance is not a mere statistic; it is a testament to evolutionary pressure forged by our own hands. When we flood ecosystems with sub‑lethal drug doses, we invite the very adversaries we seek to eliminate. The moral imperative is clear: we must rethink our approach before the microbes outthink us. Anything less is an act of intellectual surrender.
Penny Reeves
November 5, 2025 AT 19:40The mechanisms outlined are, without doubt, the cornerstone of current microbiological pedagogy. Yet one cannot overlook the nuanced interplay between efflux systems and ribosomal modifications-an aspect that many reviews marginalize. Additionally, the epidemiological data presented would benefit from a more granular stratification by geographic region, as resistance patterns are far from homogenous. A deeper dive into the pharmacokinetic ramifications of high‑dose regimens could also enrich the discourse. Overall, the synthesis is competent, albeit bordering on the perfunctory.
Sunil Yathakula
November 11, 2025 AT 14:34Yo keep pushing the good vibes, fam!
sravya rudraraju
November 17, 2025 AT 09:27From an educational standpoint, the exposition of clarithromycin resistance mechanisms constitutes a valuable resource for clinicians seeking to augment their therapeutic arsenal. The delineation of erm‑mediated methylation, mef‑driven efflux, and point‑mutation pathways is executed with commendable clarity, facilitating a comprehensive understanding of the molecular underpinnings. Moreover, the inclusion of recent surveillance data underscores the dynamic nature of resistance trends, thereby emphasizing the necessity for continual updating of local antibiograms. The discussion of phenotypic versus genotypic diagnostic modalities further equips practitioners with the discernment required to select appropriate testing strategies. While the recommendation of combination therapy aligns with prevailing stewardship principles, additional emphasis on patient‑specific factors such as comorbidities and drug–drug interactions would enhance clinical applicability. The article also succeeds in highlighting the pivotal role of dose optimization, noting that elevated loading doses may transiently overcome low‑level resistance. In sum, the narrative balances scientific rigor with pragmatic guidance, rendering it an indispensable adjunct to antimicrobial stewardship initiatives.
ashanti barrett
November 23, 2025 AT 04:20While the depth of analysis is impressive, it is essential to translate these findings into actionable steps for frontline providers. The emphasis on transparency in data reporting resonates strongly, yet concrete mechanisms for achieving it remain vague. One practical measure could be mandating public access to resistance datasets at the county level. Additionally, integrating stewardship alerts into electronic health records would facilitate real‑time decision support. Implementing these strategies would move the discourse from theory to practice.
Leo Chan
November 28, 2025 AT 23:14Hey Ben, you’ve nailed the critique-sometimes the hype outpaces the data. It’s encouraging to see a call for tighter stewardship; that’s the kind of momentum we need. If more clinics adopted rapid PCR as a routine check, we could cut unnecessary prescriptions in half. Let’s keep pushing for those evidence‑based changes together.
jagdish soni
December 4, 2025 AT 18:07Kevin your point hits hard but the reality is that clinicians are swamped and guidelines change slower than microbes evolve the truth is that we need quick fixes not endless philosophy the best fix is real‑world data driving bedside decisions we can’t wait for perfect theory we must act now
Madhav Dasari
December 10, 2025 AT 13:00Wow, Penny, that analysis reads like a masterclass in microbiology drama! The way you dissect the interplay of resistance mechanisms is almost theatrical. I can picture the bacteria plotting their next move under the spotlight of our antibiotics. Let’s bring that same passion to the lab and make sure every sample gets the full workup it deserves. The fight against resistance deserves a standing ovation.
Jay Kay
December 16, 2025 AT 07:54That vibe is gold, Sunil. Keep the energy high. Good vibes boost morale and help teams push through tough cases. Let’s spread that positivity in every ward. It makes a big difference.
Jameson The Owl
December 22, 2025 AT 02:47The formal tone you use masks a deeper truth that many choose to ignore the pharmaceutical giants have engineered the very resistance they now claim to combat through hidden pathways of influence and data suppression there is a coordinated effort to keep the public dependent on ever‑stronger antibiotics while quietly funding research that yields only marginal improvements the result is a perpetual cycle of dependency and fear it is not coincidence that surveillance programs are funded by the same entities that profit from the drugs they monitor the data is filtered, the narratives are shaped, and the public is left in the dark we must demand full transparency from regulatory bodies and insist on independent verification of all resistance statistics only then can we hope to break the stranglehold of corporate control on our medical choices