High cholesterol isn’t just a number on a lab report-it’s a silent threat that can lead to heart attacks, strokes, and blocked arteries. For millions of people, the first line of defense is a statin. But what if statins don’t work for you? Or cause muscle pain, fatigue, or other side effects? You’re not alone. About 1 in 5 people who start statins stop taking them within a year, not because they don’t work, but because they can’t tolerate them. That’s when alternatives come into play.
How Statins Actually Work
Statins aren’t just cholesterol blockers-they’re precision tools. They target an enzyme in your liver called HMG-CoA reductase, which your body uses to make cholesterol. When this enzyme is slowed down, your liver produces less cholesterol. In response, your liver pulls more LDL (the ‘bad’ cholesterol) out of your bloodstream to use for its own needs. The result? LDL levels drop-sometimes by more than 50%.
Not all statins are the same. Atorvastatin (Lipitor) and rosuvastatin (Crestor) are the most potent, often used for people with very high cholesterol or existing heart disease. Simvastatin and lovastatin are older and less powerful, but cheaper. Pravastatin and rosuvastatin are less likely to interact with other medications because they don’t rely on the CYP3A4 liver enzyme pathway. That’s important if you’re taking blood pressure meds, antibiotics, or even grapefruit juice-some statins can have dangerous interactions.
One thing to know: doubling your statin dose doesn’t double the effect. Going from 20mg to 40mg of atorvastatin might only drop your LDL another 6%. That’s why doctors don’t just keep cranking up the dose-they look for other options.
Why People Stop Taking Statins
The most common reason? Muscle pain. It’s not always obvious. You might think it’s just aging, or that you’re out of shape. But if your muscles ache, feel weak, or cramp up after starting a statin, it could be statin-associated muscle symptoms (SAMS). Studies show 5-10% of people experience this at standard doses. In rare cases, it can lead to a serious condition called rhabdomyolysis, but that’s extremely uncommon.
Some people report brain fog or fatigue. Others worry about diabetes risk-statins can slightly raise blood sugar, especially in people already at risk. But here’s the thing: the heart benefits far outweigh the risks for most people. The Cholesterol Treatment Trialists’ Collaboration found that for every 1 mmol/L (39 mg/dL) drop in LDL, the risk of heart attack or stroke drops by about 20%. That’s a huge win.
Still, if you’re one of the people who can’t tolerate statins, you need options. And you have them.
Ezetimibe: The Gentle Alternative
Ezetimibe (Zetia) works differently. Instead of stopping your liver from making cholesterol, it stops your gut from absorbing it. About 15-22% of the cholesterol you eat gets blocked from entering your bloodstream. That means less cholesterol reaches your liver, so it pulls more LDL out of your blood.
As a standalone, ezetimibe lowers LDL by about 18%. Not as strong as a statin, but it’s gentle. Many people who can’t take statins tolerate ezetimibe just fine. It doesn’t cause muscle pain. No liver enzyme spikes. No drug interactions to worry about.
But here’s where it shines: when combined with a low-dose statin. Studies show adding ezetimibe to a statin can drop LDL another 20-25%. One patient in Sydney told me, “Zetia alone got my LDL from 190 to 160. But when I added it to my low-dose simvastatin, it dropped to 110.” That’s the kind of result that keeps people on treatment.
PCSK9 Inhibitors: The Power Players
If you’ve got heart disease, diabetes, or extremely high LDL-like over 190 mg/dL-and statins aren’t cutting it, PCSK9 inhibitors might be the answer. These are injectable drugs: alirocumab (Praluent) and evolocumab (Repatha).
They work by blocking a protein called PCSK9, which normally tells your liver to destroy LDL receptors. When PCSK9 is blocked, your liver keeps more receptors alive, and those receptors pull more LDL out of your blood. The result? LDL drops by 50-60%-sometimes more.
That’s not just a number. In people with existing heart disease, PCSK9 inhibitors reduce the risk of heart attack, stroke, or death by 20%. And unlike statins, they don’t raise the risk of hemorrhagic stroke. That’s critical for people who’ve had a brain bleed in the past.
The downside? Cost and needles. These drugs cost about $5,850 a year. Insurance often denies coverage unless you’ve tried and failed on at least two statins and ezetimibe. And you have to inject yourself every two or four weeks. Some people hate needles. Others find it manageable after a few tries.
One Reddit user wrote: “Repatha lowered my LDL from 220 to 60 in three months. But my insurance denied it three times.” That’s not unusual. But for high-risk patients, it’s often worth fighting for.
Bempedoic Acid: The New Kid on the Block
Approved in 2020, bempedoic acid (Nexletol) is a newer oral option. It works in the liver, like statins, but in a different spot-on an enzyme called ACL. That means it doesn’t get into your muscles, so muscle pain is rare.
As a standalone, it lowers LDL by about 17%. When paired with ezetimibe, it can drop LDL by 35-40%. It’s not as powerful as a PCSK9 inhibitor, but it’s much cheaper and easier to take.
It’s not perfect-it can slightly raise uric acid levels, which might trigger gout in some people. But for someone who can’t take statins and doesn’t want injections, it’s a solid middle ground.
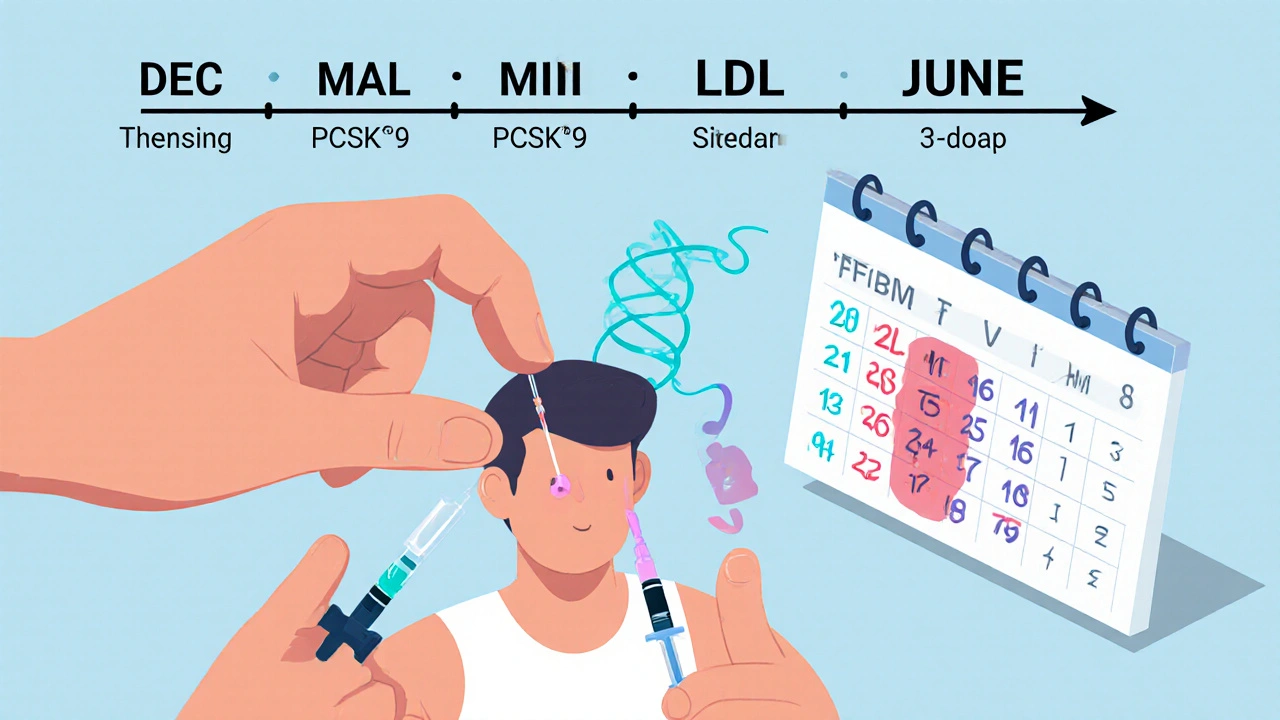
Inclisiran: The Twice-a-Year Shot
Then there’s inclisiran (Leqvio), approved in late 2021. This isn’t a traditional drug-it’s a small interfering RNA (siRNA) therapy. It turns off the gene that makes PCSK9. One shot, and your liver stops making PCSK9 for months.
You get two injections a year-once in December, once in June. It lowers LDL by 40-50%, especially when combined with a statin. No daily pills. No weekly shots. Just two quick visits to your doctor.
It’s not cheap, but it’s cheaper than monthly PCSK9 inhibitors. And for people who struggle with adherence, it’s a game-changer. Imagine not having to think about your cholesterol medication for six months at a time.
What About Supplements?
You’ve probably seen ads for red yeast rice, fish oil, plant sterols, or garlic pills that claim to lower cholesterol. Some do-slightly. Red yeast rice contains a compound similar to lovastatin, so it can lower LDL, but it’s unregulated. That means you don’t know how much active ingredient you’re getting. Some batches are dangerous.
Fish oil helps with triglycerides, not LDL. Plant sterols can lower LDL by 5-10%, but you’d need to eat fortified foods daily-like special margarine or orange juice. And even then, it’s not enough for high-risk people.
Harvard Health put it bluntly: “Statins lower harmful LDL cholesterol better than dietary supplements.” If you’re trying to avoid a heart attack, don’t gamble with supplements. They’re not replacements. They’re snacks-not meals.
How Doctors Decide What’s Right for You
Your doctor doesn’t just pick a drug. They look at your risk.
- If you’ve had a heart attack or stroke, you need strong LDL lowering-usually a high-intensity statin, maybe with ezetimibe or a PCSK9 inhibitor.
- If you have diabetes and high LDL, statins are still first choice, but if you can’t take them, bempedoic acid or ezetimibe are next.
- If you’re at moderate risk and just have high cholesterol, a low-dose statin plus lifestyle changes is usually enough.
- If you have muscle pain on statins, try switching to pravastatin or rosuvastatin. Or go to a lower dose every other day. Many people find relief without switching drugs.
- If you’ve had a brain hemorrhage, PCSK9 inhibitors may be safer than statins.
Most doctors will try two different statins before moving to alternatives. Why? Because 70% of people who quit statins because of side effects can actually tolerate a different one.
What to Expect When Starting a New Medication
Statins take 4-12 weeks to reach full effect. So don’t panic if your next blood test doesn’t show a big drop right away. Ezetimibe and bempedoic acid work at a similar pace. PCSK9 inhibitors and inclisiran show results faster-sometimes in 4-6 weeks.
Lab tests? Your doctor will check liver enzymes before starting a statin, and maybe again after a few months. But routine monitoring isn’t needed anymore unless you have symptoms. For PCSK9 inhibitors and inclisiran, no liver tests are required.
Side effects? Watch for muscle pain, dark urine, or extreme fatigue-those are red flags. For PCSK9 inhibitors, injection site reactions (redness, itching) are common but mild.
Real Talk: Access, Cost, and Sticking With It
Statins are cheap. Generic atorvastatin costs as little as $4 a month. Ezetimibe is around $20. Bempedoic acid is $100-$200. PCSK9 inhibitors? $5,000+. Inclisiran? Around $4,000 a year.
Insurance coverage varies wildly. Some require prior authorization, proof of statin failure, or even a letter from your cardiologist. If you’re denied, appeal. Many people get approved on the second try.
And adherence matters. Taking your meds every day-even if you feel fine-is what keeps your arteries clear. Missing doses is like leaving your front door open. The cholesterol sneaks back in.
Support helps. The American Heart Association’s ‘Check. Change. Control.’ program gives free tools. Your pharmacist can help you set up pill reminders. Talk to others on patient forums-just don’t let anecdotal stories replace medical advice.
Final Thoughts: There’s No One-Size-Fits-All
Statins are the foundation. They’ve saved millions of lives. But they’re not the only tool in the box. If they don’t work for you, it’s not failure-it’s a chance to find a better fit.
Whether it’s ezetimibe for gentle lowering, bempedoic acid for muscle-sensitive patients, PCSK9 inhibitors for high-risk cases, or inclisiran for those who hate daily pills-there’s a path forward. The goal isn’t just to lower a number. It’s to live longer, healthier, and free from the fear of a heart attack.
Your cholesterol isn’t your enemy. It’s a signal. Listen to it. Work with your doctor. And don’t give up if the first option doesn’t stick.

Ravinder Singh
November 19, 2025 AT 15:14Statins saved my dad’s life after his angioplasty 😊 But when he got muscle pain, we thought it was over… until we found ezetimibe. Now he’s cruising at LDL 90, no aches, no stress. Sometimes the fix isn’t stronger-it’s smarter. Glad this post laid it all out. 💪
Russ Bergeman
November 21, 2025 AT 11:41Statins are overhyped. My LDL was 210-I ate avocado toast, took garlic pills, and now it’s 180. Who needs pharma when you’ve got brunch? 🥑
Dana Oralkhan
November 22, 2025 AT 05:02I just want to say-this post is so thoughtful. So many people feel alone when they can’t tolerate statins. But you’re not broken. You’re just on a different path. Ezetimibe, bempedoic acid, inclisiran-they’re not second choices. They’re valid, powerful tools. And your worth isn’t tied to your LDL number. ❤️
Jeremy Samuel
November 24, 2025 AT 01:19statins r a scam lol. my uncle took em for 5 yrs and still had a heart attack. now he eats butter and calls it ‘ancestral healing’. he’s 78 and rides his bike daily. who’s the real genius here? 🤷♂️
Destiny Annamaria
November 24, 2025 AT 22:38OMG I’m so glad someone finally said this!! I’m a yoga instructor in Austin and half my students are on statins. One girl cried because her insurance denied Repatha. We started a GoFundMe for her. We’re all just trying to live, ya know? 💕
Ron and Gill Day
November 25, 2025 AT 01:23This article is a pharmaceutical marketing brochure. PCSK9 inhibitors cost $5,850? That’s robbery. And you’re telling people to ‘fight for coverage’? Meanwhile, real people are choosing between insulin and groceries. This isn’t medicine-it’s capitalism with a stethoscope.
Alyssa Torres
November 26, 2025 AT 11:49I have familial hypercholesterolemia. I was on a high-dose statin for 3 years-muscle pain so bad I couldn’t lift my coffee cup. Then I tried inclisiran. Two shots a year. No daily pills. My LDL dropped from 240 to 65. I cried the first time I saw the lab results. This isn’t just medicine-it’s freedom. 🙏
Summer Joy
November 27, 2025 AT 13:59Okay but… what if you’re just lazy? Like… why not just eat less cheese? Why do you need a $4000 shot? 😭
Aruna Urban Planner
November 28, 2025 AT 10:44The pharmacoeconomic dissonance here is noteworthy. While statins exhibit cost-effectiveness ratios under $10,000/QALY, PCSK9 inhibitors exceed $150,000/QALY-raising ethical concerns regarding distributive justice in public health systems. The biopolitical framing of ‘adherence’ often obscures structural barriers to care.
Nicole Ziegler
November 29, 2025 AT 04:06incli-siran?? 🤯 two shots a year?? i’m sold. also… anyone else feel like cholesterol is just society’s way of making us feel guilty for eating pizza? 🍕
Bharat Alasandi
November 30, 2025 AT 22:52bro i was on simvastatin, got so tired i napped after walking to fridge. switched to bempedoic acid + ezetimibe. no muscle pain, no brain fog. my doc said ‘you’re one of the lucky ones’. honestly? i just want to live long enough to see my nephew graduate. 🙏
Kristi Bennardo
December 2, 2025 AT 20:24This article is dangerously misleading. It implies that pharmaceutical alternatives are equally efficacious. The clinical data does not support this. Statins remain the gold standard. To suggest otherwise is irresponsible. Patients deserve evidence-not anecdotes.
Shiv Karan Singh
December 3, 2025 AT 05:38LOL you guys are all so naive. Statins cause cancer. I read it on a forum. Also, cholesterol is not bad-it’s your body’s natural armor. Eat butter. Lift weights. Ignore doctors. 🧠🔥