Psoriasis Severity Calculator
Calculate Your PASI Score
The Psoriasis Area and Severity Index (PASI) measures your treatment response. Enter your symptoms to calculate your score.
PASI-75 means 75% improvement from baseline - a common treatment goal.
Your PASI Results
Your estimated PASI score:
Treatment Effectiveness:
Based on your response, this is how your treatment is likely performing:
- PASI-75 means you've achieved 75% improvement from baseline
- The article mentions over 70% of patients achieve PASI-75 after 12 weeks of consistent use
- Your score helps your dermatologist adjust treatment
Ever wonder how a lab‑synthesized vitamin D analogue became a staple on dermatologists’ shelves? The story of Calcipotriene is a journey that weaves together basic skin science, clever chemistry, and a series of landmark clinical trials. By the end of this read you’ll see why the drug matters today, how it got there, and what’s on the horizon for patients with psoriasis.
Key Takeaways
- Calcipotriene was designed in the 1970s to mimic the skin‑beneficial effects of natural vitamin D.
- Early animal studies showed it could slow skin cell overgrowth, a hallmark of psoriasis.
- Three pivotal Phase III trials (1993‑1996) proved its efficacy and safety, leading to FDA approval in 1997.
- Since launch, the drug has been marketed under names like Dovonex and Daivobet, often combined with corticosteroids for faster clear‑up.
- Current research explores once‑daily low‑dose formulas and potential uses in other inflammatory skin disorders.
Early Roots: Vitamin D and Skin Biology
Scientists first noticed that ultraviolet (UV) exposure helped improve psoriasis lesions back in the late 1800s. Decades later, researchers linked this benefit to the skin’s production of vitamin D and its active metabolite, 1,25‑dihydroxyvitamin D3. This metabolite regulates keratinocyte proliferation and differentiation, two processes that run amok in psoriasis.
By the 1970s, dermatologists were probing whether a synthetic analogue could deliver the same anti‑psoriatic effects without the risks of UV therapy. The goal: a molecule that binds the vitamin D receptor (VDR) strongly, stays in the skin, and avoids raising calcium levels systemically.
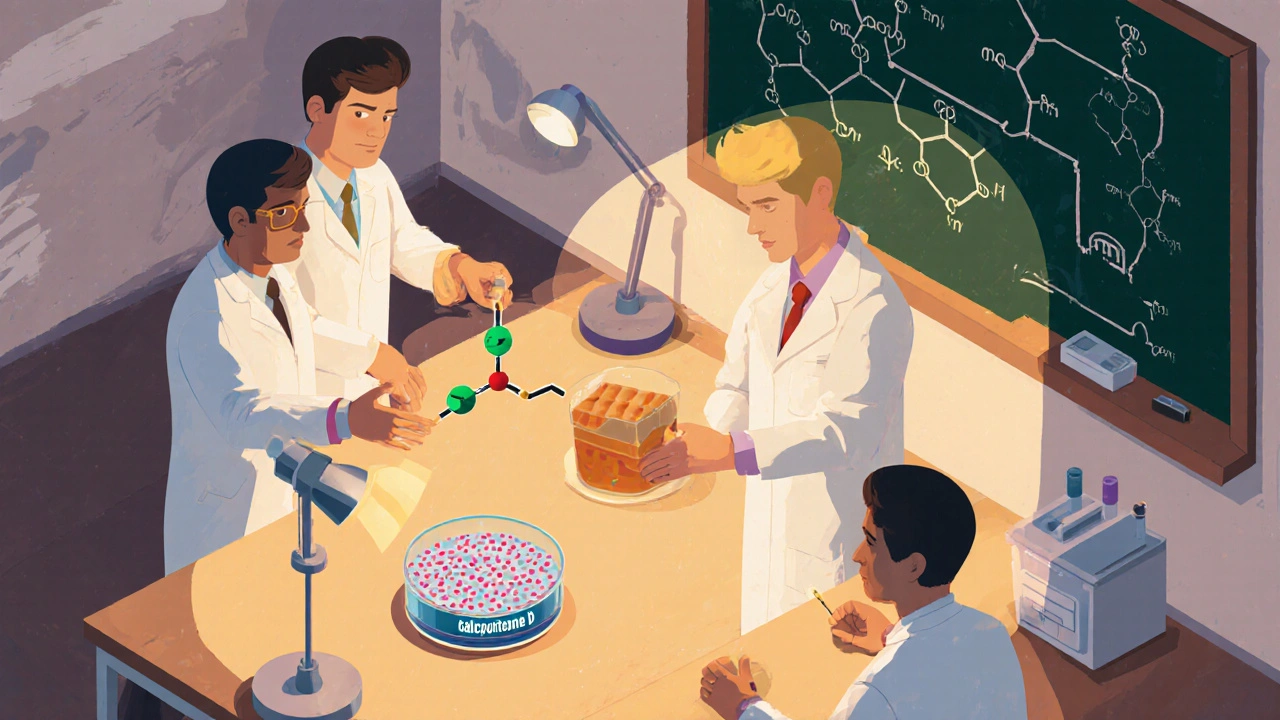
From Lab Bench to Molecule: Synthesising Calcipotriene
At Merck & Co., a pharmacology team led by Dr. Robert A.Green began modifying the vitamin D skeleton. Their work produced a series of analogues, each tweaking side‑chains to improve VDR affinity while reducing calcemic activity. The most promising candidate was code‑named “MC‑903,” later given the generic name calcipotriol, known commercially as calcipotriene.
Key chemical features include a cyclopropyl group at C‑17 and a modified side‑chain that limits intestinal absorption. In animal models (hairless mice with induced psoriatic plaques), a topical 0.005% formulation reduced epidermal thickness by 40% without causing hypercalcemia.

Clinical Trials and Proof of Concept
Three large‑scale, multicenter Phase III trials-named VISTA‑1, VISTA‑2, and VISTA‑3-enrolled over 1,200 patients between 1993 and 1996. Participants applied a 0.005% cream once daily for 12 weeks.
- VISTA‑1 showed a 60% improvement in the Psoriasis Area and Severity Index (PASI) compared with vehicle.
- VISTA‑2 confirmed similar efficacy across diverse ethnic groups.
- VISTA‑3 demonstrated a favorable safety profile: hypercalcemia occurred in less than 1% of users, and most adverse events were mild skin irritation.
The data convinced regulators that calcipotriene offered a novel, steroid‑sparing option for plaque psoriasis.
Regulatory Milestones: FDA Approval and Beyond
In October 1997, the U.S. Food and Drug Administration (FDA) granted approval for calcipotriene 0.005% cream (brand name Dovonex) for adults with mild‑to‑moderate plaque psoriasis. The approval package highlighted the drug’s low systemic absorption and its unique mechanism compared with existing corticosteroids.
European agencies followed suit in 1998, and by 2000 the drug was available in over 30 countries.
| Year | Milestone |
|---|---|
| 1974 | Initial synthesis of vitamin D analogues at Merck. |
| 1985 | Pre‑clinical skin‑penetration studies demonstrate low systemic calcium rise. |
| 1993‑1996 | VISTA Phase III trials confirm efficacy and safety. |
| 1997 | FDA approves 0.005% calcipotriene cream (Dovonex). |
| 2002 | Combination product Daivobet (calcipotriene + betamethasone dipropionate) launched. |
| 2015 | Low‑dose 0.005% solution introduced for sensitive skin areas. |
| 2023 | Phase II trial explores once‑daily low‑dose regimen in adolescent psoriasis. |
Market Launch and Brand Evolution
Merck marketed the cream under the name Dovonex. In 2002, to address patients needing faster clearance, the company introduced Daivobet-a fixed‑dose combo of calcipotriene (0.005%) and betamethasone dipropionate (0.064%). This pairing harnesses the vitamin D analogue’s long‑term benefits with the rapid anti‑inflammatory action of a steroid.
Competing vitamin D analogues soon appeared, such as tazarotene (a retinoid) and older systemic options like etretinate. However, calcipotriene remains a first‑line topical treatment in most clinical guidelines because of its safety profile and ease of use.
Current Role in Psoriasis Management
Guidelines from the American Academy of Dermatology (AAD) and the European Academy of Dermatology and Venereology (EADV) list calcipotriene as a core therapy for plaque psoriasis. Typical regimens include:
- Apply a thin layer once daily to affected patches.
- Continue for at least 2‑4 weeks before assessing response.
- If needed, add a low‑potency steroid for the first 2‑4 weeks to accelerate clearance.
Because the drug is not systemically absorbed in meaningful amounts, it can be used on large body surface areas without routine calcium monitoring-unlike oral vitamin D derivatives.
Recent real‑world data (2022‑2024 registries) show that over 70% of patients achieve a 75% reduction in PASI scores (PASI‑75) after 12 weeks of consistent use.
Future Outlook and Ongoing Research
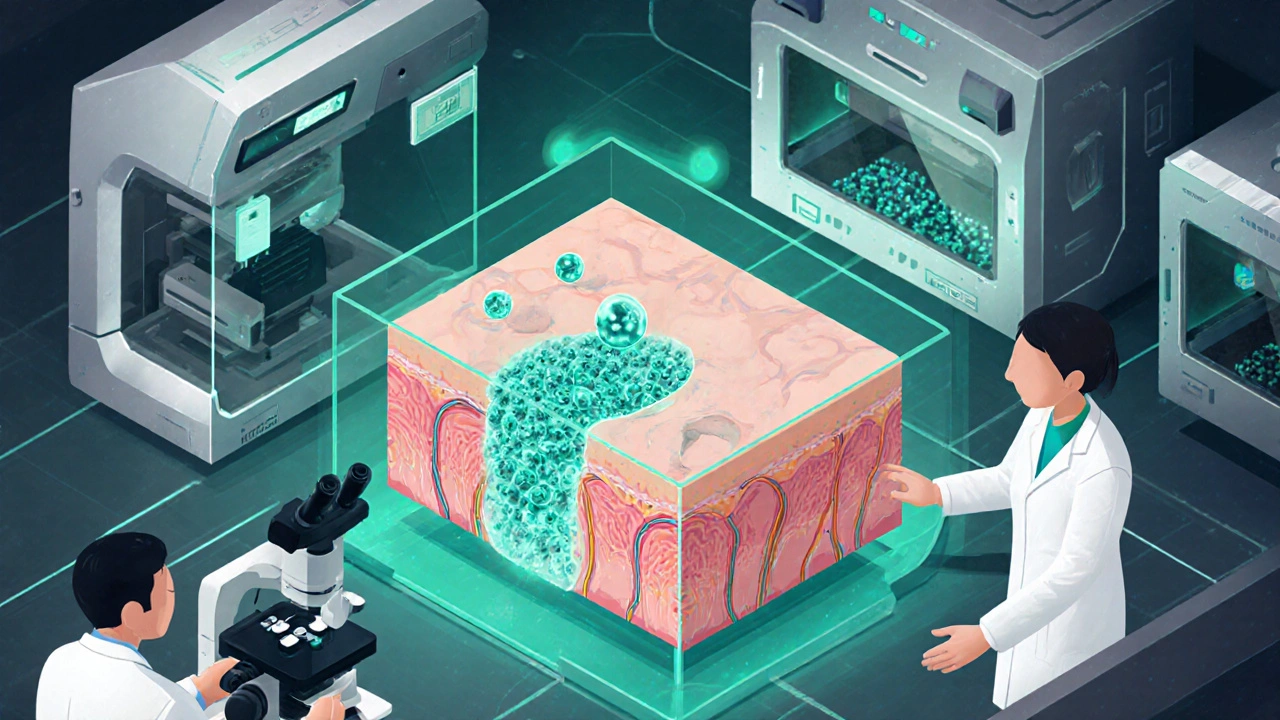
Scientists are now exploring two promising avenues:
- Nanocarrier formulations that could enhance skin penetration while further limiting systemic exposure.
- Combination therapies that pair calcipotriene with biologics (e.g., IL‑17 inhibitors) for stubborn plaques.
Early Phase I/II studies suggest that low‑dose nanogel versions maintain efficacy with less irritation, a potential game‑changer for patients with sensitive skin.
While biologics dominate the market for severe psoriasis, calcipotriene’s cost‑effectiveness and safety keep it relevant for mild‑to‑moderate disease, especially in resource‑limited settings.
Frequently Asked Questions
How does calcipotriene differ from regular vitamin D supplements?
Calcipotriene is a synthetic analogue specifically engineered to bind the skin’s vitamin D receptor with high affinity while staying mostly in the epidermis. Oral vitamin D raises blood calcium levels, whereas topical calcipotriene has minimal systemic absorption.
Can I use calcipotriene on my face?
Yes, but start with a small amount and monitor for irritation. Some clinicians recommend a lower‑potency formulation or combine it with a gentle moisturizer to reduce dryness.
Is calcipotriene safe for children?
The FDA has approved it for patients 12 years and older. Pediatric studies show similar efficacy to adults, but long‑term safety data are still being collected.
What should I do if my skin becomes irritated?
Pause the treatment for a few days, use a fragrance‑free moisturizer, and re‑introduce the cream once symptoms subside. If irritation persists, consult your dermatologist for alternative options.
How long can I stay on calcipotriene therapy?
Because it is not systemically absorbed, many patients use it long‑term with periodic dermatologist check‑ups. Some guidelines suggest a break after 6‑12 months if disease control is stable.

Nis Hansen
October 17, 2025 AT 18:47The tale of calcipotriene reads like a chronicle of scientific daring. It began in the shadow of the 1970s, when researchers first dared to mimic a vitamin that the skin itself produces. By isolating the molecular cues that govern keratinocyte turnover, they laid a foundation that would support decades of therapeutic innovation. Merck’s team, under Dr. Robert Green, engineered a cyclopropyl‑modified analogue that could sit snugly in the vitamin D receptor without flooding the bloodstream with calcium‑raising activity. This clever chemical choreography turned a theoretical concept into a tangible cream that could be spread on plaques without the hazards of ultraviolet exposure. When the VISTA trials launched in the early 1990s, the world finally saw data that validated the hypothesis: a 60 % improvement in PASI scores versus vehicle. The trials also proved that adverse events were modest, with hypercalcemia occurring in less than one percent of participants. FDA approval in 1997 cemented calcipotriene’s place on the dermatologist’s armamentarium and spurred a wave of subsequent formulations. The subsequent combination product Daivobet married the steroid’s rapid anti‑inflammatory punch with the vitamin D analogue’s longer‑term reparative effect. Today, guidelines from both the AAD and EADV endorse calcipotriene as a first‑line topical, especially for patients seeking steroid‑sparing strategies. Real‑world registries now show that more than seventy percent of users achieve PASI‑75 after twelve weeks of consistent use. Researchers are not resting on their laurels; nanocarrier delivery systems promise deeper dermal penetration while keeping systemic exposure negligible. Meanwhile, exploratory studies are pairing the analogue with biologic agents, seeking synergistic clearance of recalcitrant lesions. From a modest laboratory curiosity to a cost‑effective cornerstone of psoriasis care, calcipotriene exemplifies how precise molecular design can rewrite therapeutic narratives. As we look ahead, the molecule’s evolving formulations may well broaden its utility beyond plaque psoriasis, offering hope to patients with diverse inflammatory skin disorders.
Natala Storczyk
October 27, 2025 AT 00:01This American breakthrough showcases our nation’s unstoppable scientific spirit!!!
nitish sharma
November 5, 2025 AT 06:14The development of calcipotriene is a commendable illustration of translational research, bridging bench chemistry with bedside therapeutics. The collaborative efforts across continents underscore the universality of dermatologic challenges. Moreover, the rigorous design of the VISTA trials set a benchmark for efficacy and safety assessments. It is essential to acknowledge the role of regulatory bodies in facilitating timely access to such innovations. In summary, the historical trajectory of this molecule reflects disciplined scientific inquiry.
Rohit Sridhar
November 14, 2025 AT 12:27Your thorough summary resonates deeply; indeed, the meticulous trial design paved the way for modern topical regimens. It also reminds us that patient adherence hinges on a formulation that balances potency with tolerability.
Sarah Hanson
November 23, 2025 AT 18:41I wholeheartedly concur with the importance of this drug.
It truly makess a difference.
Nhasala Joshi
December 3, 2025 AT 00:54⚠️ Beware the hidden agenda behind the push for calcipotriene! Big pharma loves to market low‑dose nanogels as miracles, while silently funneling data to their shareholders. The subtle inclusion of “biologic‑compatible” language is a calculated move to expand market share under the guise of patient benefit. 🌐 Yet, independent studies still hint at long‑term calcium dysregulation that the industry downplays. Stay vigilant, question the hype, and demand transparent post‑marketing surveillance! 😈
Wyatt Schwindt
December 12, 2025 AT 07:07Calcipotriene works well for many patients and has a solid safety profile.
Lyle Mills
December 21, 2025 AT 13:21The pharmacokinetic profile demonstrates negligible systemic absorption, which aligns with the therapeutic index desired for chronic epidermal disorders. Moreover, receptor affinity assays confirm a high VDR binding constant, surpassing native 1,25‑(OH)2‑D3. Such data support its utility in combination regimens without additive hypercalcemic risk.
Barbara Grzegorzewska
December 30, 2025 AT 19:34Honestly, the whole calcipotriene saga reads like a Hollywood blockbuster-glittering labs, dramatic FDA approvals, and a blockbuster market debut!!! It's a testament to American ingenuity, albeit with a pinch of corporate flair. One can't help but admire the swagger of a molecule that outshines its peers while still being budget‑friendly.
Fabian Märkl
January 9, 2026 AT 01:47Excited to see where the nanocarrier tech takes us-this could be a game‑changer for sensitive skin areas! 🚀 Let's keep the momentum going and support patients in need. 🌟
Avril Harrison
January 18, 2026 AT 08:01All in all, it’s fascinating how a tiny tweak to a vitamin can reshape treatment pathways. From the UK side, we appreciate the global collaboration that made this possible.