Antihistamine Risk Calculator
This tool helps you understand your risk of anticholinergic side effects from first-generation antihistamines based on your health factors. Note: Second-generation antihistamines (cetirizine, loratadine, fexofenadine) carry significantly lower risk.
Risk Level:
Most people reach for antihistamines when their allergies act up. They grab a bottle of Benadryl or a generic diphenhydramine tablet, swallow it, and expect relief from sneezing and itchy eyes. What they don’t realize is that the same pill that stops their runny nose might also be causing dry mouth, trouble going to the bathroom, or even difficulty urinating. These aren’t random side effects-they’re direct results of something called anticholinergic effects.
What Exactly Are Anticholinergic Effects?
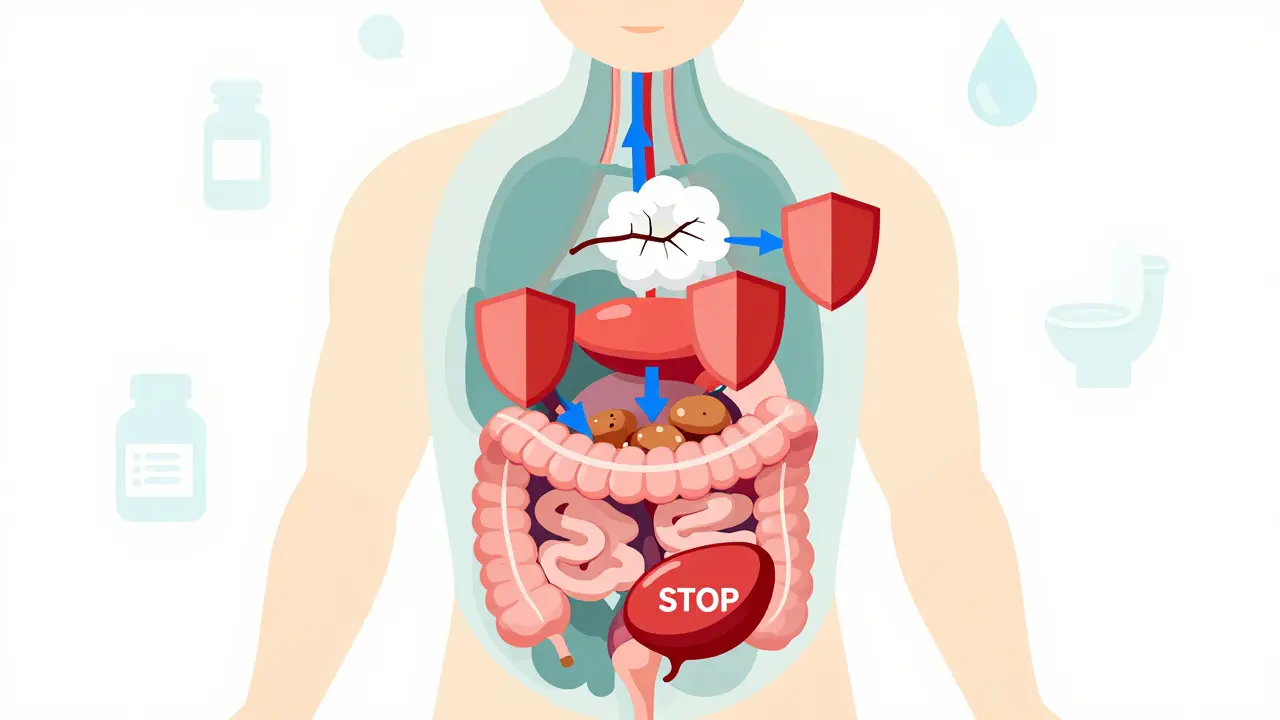
Anticholinergic effects happen when a drug blocks acetylcholine, a chemical in your body that tells muscles and glands what to do. Histamine blockers like diphenhydramine, chlorpheniramine, and promethazine were designed to stop histamine, the trigger for allergy symptoms. But because of how they’re built, they accidentally latch onto muscarinic receptors too-those are the ones that respond to acetylcholine. When that happens, your body’s normal signals get scrambled.Think of it like turning off a light switch that controls more than one bulb. You only meant to turn off the kitchen light, but now the bathroom light, the hallway light, and the porch light are out too. That’s what antihistamines do to your nervous system. The result? Three common, often ignored, side effects: dry mouth, constipation, and urinary issues.
Dry Mouth: More Than Just Uncomfortable
If you’ve ever taken a first-generation antihistamine and felt like your mouth had been stuffed with cotton, you’re not imagining it. Studies show these drugs can slash saliva production by 60-70%. That’s not just annoying-it’s risky. Saliva isn’t just there to help you swallow. It protects your teeth, washes away bacteria, and keeps your mouth from getting infected.People on diphenhydramine report needing to sip water constantly. Some even wake up at night with cracked lips or a sore throat. Over time, chronic dry mouth increases the chance of cavities, gum disease, and oral thrush. The American Dental Association recommends chewing sugar-free gum with xylitol to help. It doesn’t fix the root cause, but it can boost saliva flow by 40-60% in minutes.
Constipation: When Your Gut Slows Down
Your digestive system relies on acetylcholine to make the muscles in your intestines contract and push food along. Block that signal, and things slow down-fast. Clinical trials show first-generation antihistamines can increase bowel transit time by 1.5 to 2 times normal. That means food sits longer, water gets pulled out, and stools become hard and difficult to pass.About 15-20% of people taking diphenhydramine regularly report constipation. For older adults or those with existing bowel issues, this isn’t just uncomfortable-it can lead to bowel obstruction or fecal impaction. The American Gastroenterological Association suggests using polyethylene glycol (17g daily) as a preventive measure if you must use these drugs. It’s not glamorous, but it cuts constipation risk from 18% down to 5% in studies.

Urinary Retention: A Serious Risk, Especially for Men
This is where things get dangerous. Acetylcholine tells your bladder to contract so you can pee. When antihistamines block that signal, your bladder doesn’t empty fully. For men with enlarged prostates, this can turn into a medical emergency. Research shows that men with an International Prostate Symptom Score above 8 have a 31% chance of acute urinary retention within 48 hours of taking a first-generation antihistamine.Women aren’t immune either. Bladder muscle weakness can lead to frequent urges, incomplete emptying, and even urinary tract infections. The American Urological Association explicitly warns against using these drugs in patients with any history of urinary retention. If you’re struggling to start peeing, feeling like you can’t fully empty your bladder, or having pain after urinating-stop the medication and talk to your doctor.
First-Generation vs. Second-Generation: The Real Difference
Not all antihistamines are created equal. The older ones-diphenhydramine, chlorpheniramine, hydroxyzine-were developed in the 1940s. They cross the blood-brain barrier easily and hit acetylcholine receptors hard. The newer ones-cetirizine (Zyrtec), loratadine (Claritin), fexofenadine (Allegra)-were designed to avoid that.Here’s what the numbers show:
| Side Effect | First-Generation (e.g., Diphenhydramine) | Second-Generation (e.g., Cetirizine, Fexofenadine) |
|---|---|---|
| Dry Mouth | 28% | 2-4% |
| Constipation | 15-20% | 3-5% |
| Urinary Retention (in elderly) | 5-8% | <1% |
| Cognitive Impact (Dementia Risk) | 54% increased risk over 7 years | No significant increase |
The difference isn’t subtle. If you’re over 65, have prostate issues, or suffer from chronic constipation, switching to a second-generation antihistamine isn’t just a smart choice-it’s a safety move.
Why Do People Still Use First-Generation Antihistamines?
You’d think everyone would switch after learning this. But here’s the catch: price and availability. A 24-dose bottle of generic diphenhydramine costs $4-6. Cetirizine or fexofenadine? $12-18. That’s a big difference if you’re paying out of pocket.Also, many people still use them as sleep aids. Diphenhydramine is in dozens of nighttime cold and allergy formulas. It works-because it makes you drowsy. But that drowsiness isn’t harmless. The American Academy of Neurology found that even short-term use (7+ days) increases fall risk by 34% in older adults. Combine that with dry mouth and urinary retention, and you’ve got a recipe for hospital visits.
Who Should Avoid These Medications Altogether?
The American Geriatrics Society’s Beers Criteria lists first-generation antihistamines as “potentially inappropriate” for people over 65. That’s not a suggestion-it’s a warning based on decades of data. The same goes for anyone with:- Enlarged prostate or urinary retention
- Chronic constipation or ileus
- Glaucoma (especially narrow-angle)
- History of dementia or cognitive decline
- Heart rhythm problems (some anticholinergics can prolong QT interval)
Even if you’re young and healthy, long-term use isn’t risk-free. A 2015 study in JAMA Internal Medicine found that people who took diphenhydramine for more than 90 doses per year over 7 years had a 54% higher risk of developing dementia. The more you take, the higher the risk. It’s not a guarantee-but it’s a clear signal.
What Should You Do Instead?
Switching to a second-generation antihistamine is the easiest fix. Cetirizine, loratadine, and fexofenadine work just as well for allergies-without the dry mouth, constipation, or urinary trouble. They last 24 hours, so you only need one dose a day. And they don’t make you sleepy (unless you’re one of the rare people who reacts to cetirizine).If you’re using an old-school antihistamine as a sleep aid, try melatonin instead. It’s not as strong, but it doesn’t mess with your nervous system. For allergies, nasal steroid sprays like fluticasone are more effective long-term than oral antihistamines anyway.
And if you’re unsure? Talk to your pharmacist. They see this every day. Ask: “Is this antihistamine likely to cause dry mouth or trouble peeing?” If they hesitate, it’s probably not the right choice.
Bottom Line
Antihistamines are useful. But not all of them are safe. The dry mouth, constipation, and urinary issues you might brush off as “just side effects” are signs your body’s signaling system is being disrupted. For most people-especially those over 65 or with existing health conditions-first-generation antihistamines do more harm than good.There’s no need to suffer through these side effects. Second-generation options exist for a reason: they work without the risks. If you’re still using Benadryl or a generic version for allergies or sleep, it’s time to reconsider. Your mouth, your gut, and your bladder will thank you.